The H5N1 virus needs several mutations to create a human pandemic
Although media headlines have noted the opposite, the H5N1 virus should carry out more than one mutation causing a human pandemic. Professor of microbiology Ignacio López-Goñi and virologist Elisa Pérez Ramírez explained this in the publication "the Conversation". In the article signed by both, detailed explanations have been given about the situation, the characteristics of the virus and how it should change so that humans could become infected, penetrate their cells and replicate. They have made it clear, for all this, that a single mutation is not enough.
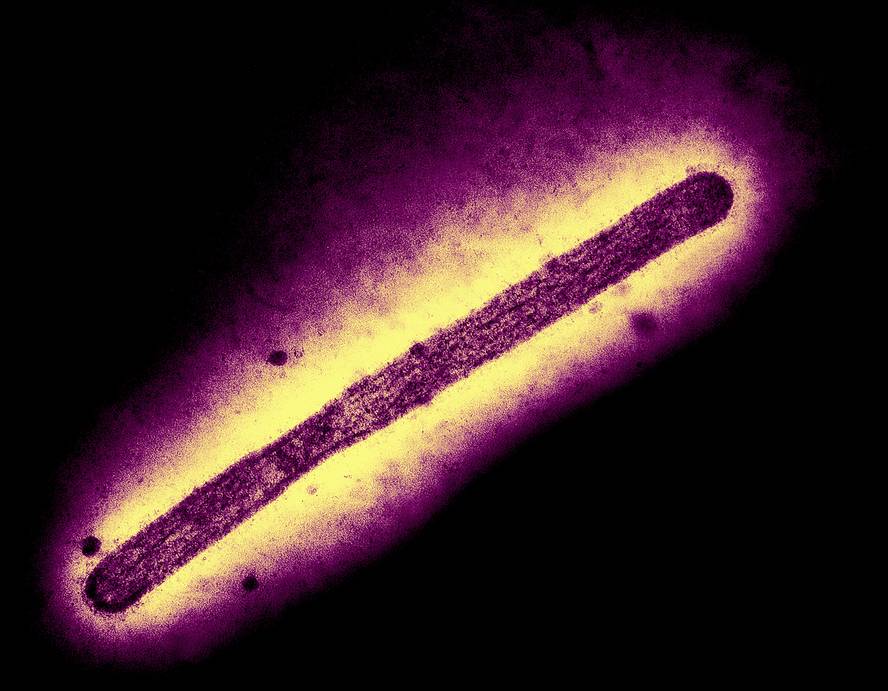
As you have explained, the misunderstanding comes from another article published in Science magazine in December 2024. In an in vitro laboratory study, researchers found that a specific mutation of a protein, haemagglutinin, from the H5N1 virus, provides the virus with a facility to bind to human receptors.
This, in a way, suggested that if the virus mutated like in the laboratory, humans would be more likely to become infected. For the time being, however, the virus does not have too many facilities to connect to human receptors. In fact, birds are the first recipients of the most widespread H5N1 variant today. In addition to the ease of connection to bird receptors, it is introduced and replicated in its cells causing them serious pathologies. Thus, worldwide, millions of birds have died from the virus. But in addition to infecting birds, it has also infected mammals. As specified by López-Goñi and Pérez, the presence of more than 350 species of birds and 50 species of mammals has been detected, that is, it has caused a panzootia.
In humans
Among mammals, cow crops have a special responsibility, as the virus has spread widely in U.S. crops and most of the infections diagnosed in people in that country have been through cows. In the article, the authors point out that a total of 64 cases have been recorded, and those that have not been caused by cows, except in a case in which it has not been possible to identify their origin, have been through domestic birds. In fact, most of the cases that have occurred in the rest of the world have been through domestic birds.
In infected people in the United States, the most common symptom has been conjunctivitis, which has affected almost all patients. Almost half of the cases have had fever, and just over a third, respiratory symptoms. The first death has recently been confirmed in the United States, in Lousiana, and in Canada there has also been another patient that has been very serious. In no case has the virus been shown to be passed from the person to the person.
With all this in mind, the authors believe that if they spread in humans, it will take longer for the virus to find the right combination of mutations. It is not enough to hold human cells well, it must be able to internalize and reproduce and overcome the immune system. As they have anticipated, part of the population is very likely to have some type 1 neuranimidase immunity, as, for example, it has contact with H1N1 flu, or seasonal vaccines can provide some kind of protection.
In any case, the title mentioned at the beginning (a single mutation is sufficient for avian influenza to give rise to a human pandemic) has been denied. But they have not concealed their concern, especially if a vulnerable species (pig, cow, mink) is simultaneously infected with human and bird flu: this situation would facilitate the reorganization of the genomes of the virus and the formation of a hybrid capable of infecting humans. To avoid this, and in order to implement effective preventive measures, López-Goñi and Pérez have supported the Unified Health Strategy.