Can cervical cancer be prevented?

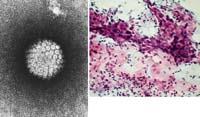
The causes of this type of cancer are viruses, human papilomabirus. Infection of these viruses is very common worldwide and causes skin and/or mucous infections. Many types of papillomavvirus or human genotypes, more than 120, are known to produce different types of infections. For example, skin warts are mainly due to genotypes 1, 2 and 4, while other genotypes cause mucosal infections. Fortunately, in mucous infections, only some of these genotypes are oncogenic (about 15 to 20). Therefore, depending on the oncogenic capacity of these viruses, we classify genotypes of different types: low-risk human papilomabiruses (genotypes 6 and 11) and high-risk human papilomabiruses (genotypes 16, 18, 31 and 45).
Human papillomaviruses that affect genital mucous membranes are transmitted through sexual intercourse. Lesions on genital skin are called acuminated condylomas and are warts, usually caused by genotype 6 or 11. These lesions may increase during pregnancy or in situations where the immune system is weakened and take the form of a cauliflower. Normally these genital infections are benign and disappear. However, sometimes other human papillomavirus can cause intrepidal neoplasms, dysplasias, and carcinoma, and cause cervical cancer. The main cause of these malignant lesions is genotype 16, although others may also participate (genotypes 18, 31 and 45).
Risk factors
The infection of human papillomavirus in genital mucous membranes and, therefore, the appearance of cancer, are factors that favor the appearance of youth and sexual relations. It is currently the most sexually transmitted infection worldwide, in addition to having a very high degree of pollution. In addition, infection is more common in people who start sexual intercourse early and especially in young women with a high number of sexual members. This is because viruses attach very well to the epithelial cells located in the cervix, due to changes that occur in adolescence itself. The incidence of infection decreases over the years and increases again in the years before and after menopause.

Other factors that influence infection are food, tobacco, changes in the immune system, infection with other infectious agents (herpes simplex or Chlamydia), multiple pregnancy, and oral contraceptives.
Symptoms
Normally, genital human papillomavirus infection does not give significant signs or symptoms at first. Infection occurs therefore during the first sexual intercourse. Subsequently, these viruses remain unexpressed, being able to remain in a state of intracellular origin for many years. In fact, since the onset of infection and the onset of malignant injury many years pass, at least 10. Therefore, cervical cancer does not appear in young girls and is more common from age 45-50. However, when some symptoms appear, some tests may be done to find out if there is an infection. Symptoms may include vaginal bleeding, abnormal vaginal discharge, pelvic pain, or pain during sex.
Prevention of congratulations
Currently, the only measure to prevent this type of cancer is a gynecological study. Tests in this study can detect the presence of infection. Some of the tests that can be done are cytology or the Pap test. These tests take cells from the surface of the cervix and are checked under a microscope for abnormal structures. However, these tests, although recommended for all women who have sex, are not performed many times, especially in undeveloped territories. Sometimes they occur when lesions appear, so when the disease appears a treatment is applied that in some cases is too late. Therefore, this prevention does not control the infection. Therefore, research and obtaining vaccines against human papilomabirus has been a great boost.
There are currently two types of vaccines for the prevention and control of cervical cancer. These prophylactic vaccines are based on the virus ( L1 virus-like particles), in fact they are formed by the virus protein L1 and have the same appearance as this, but by not containing the virus genome they cannot cause the disease. They are very immunogenic, so they stimulate the formation of antibodies and thus manage to protect them.

The first vaccine, called Gardasil (Sanofi Pasteur MSD), is made with four types of human papillomavvirus (16, 18, 6 and 11), while the second, called Cervarix (from the GSK house), consists only of two genotypes (16 and 18). At the moment, the only one recognized worldwide is the first, because the other still has to pass some tests to market it.
Knowing that most cervical cancers (70%) are due to genotypes 16 and 18 and that 90% of genital warts are due to types 6 and 11, it seems that this prophylactic vaccine that exists on the market will be very successful. In addition, according to the latest studies, once administered this vaccine not only reduces the infection of these genotypes, but also of other genotypes (31, 45, ..). This is because cross-reactions occur.
Knowing when human papillomavirus infection starts, it seems that it would be best for the vaccine to get into contact with the virus, that is, before having sex. Therefore, the most convenient would be for girls to integrate before adolescence and adolescence (between 9 and 13 years). Preventive vaccination of cervical cancer has been carried out in most EU territories since the beginning of this year. In our territory, Osakidetza has approved the implementation of this vaccination program and recently announced that the vaccination campaign will begin this year, in fact the Gardasil vaccine is already in pharmacies. Here girls ages 11 to 13 will be vaccinated in three doses.

The implementation of an effective vaccination program for human papillomavirus would reduce mortality not only in our territory, but also in undeveloped territories, and in particular in them, and, moreover, reduce health costs, since cytology production should be reduced.





