Pacemaker: tired heart guide
The battery, which originated an initial stimulus, and the cable that led this stimulus to the heart, formed the pacemaker, while today, as electronic circuits have developed, the functions that this apparatus can perform have increased considerably. The battery and cables have also known significant progress. As materials for electrode manufacturing have been modified and improved, the reliability of the appliance has also increased and its duration has increased considerably.
The batteries were initially mercury and large, so because of their short duration, it was very difficult to use patients as stents. After passing through the atomic plutonium batteries, lithium batteries are currently used; in addition to storing a lot of energy in a very small volume, when they are about to run out, the voltage jump does not occur suddenly, so they allow to change patients before they present symptoms. The development that has occurred in recent years in microprocessors will be analyzed later, after analyzing the operation of pacemakers.
Heart: muscle that contracts rhythmically
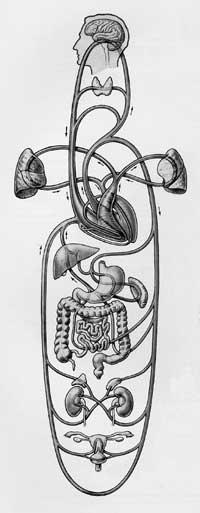
The main function of the heart is to pump blood to the whole body. To achieve this goal, this muscle, divided into four main chambers, works synchronously. In blood transit two circuits can be distinguished. After the absorption of oxygen by the blood of the organs of the body, the venous system reaches the right atrium.
From there, the right ventricle and its pump function allow it to move to the lungs, where, once oxygen is saturated, it is directed towards the left atrium. It passes to the left ventricle that sends it to the whole body by closing the second circuit. Both atria contract simultaneously to facilitate the passage of blood to the ventricles, and the two ventricles contract simultaneously directing blood to each of the circuits. But what causes the rhythmic contraction of the heart?
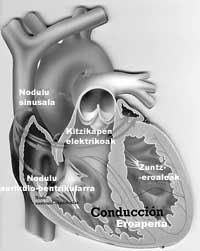
The phenomenon described is due to the electrical excitation that occurs in the heart itself. External quinadas (nervous system, hormones, etc.) can alter their frequency, but under normal conditions is generated by a group of cells located in the right atrium. Due to their physiological characteristics, these cells that form the sinus node generate 70 impulses per minute. Through specific conduction systems, a second nodule, the atrioventricular node, is passed between the atria and ventricles. Then, when it spreads to the two ventricles, they contract and send blood. The sinus node is therefore the physiological pacemaker of the heart.
Slow rhythms, pacemaker signal
When the sinus node is not able to perform its function, the substitutes are ordered, but always less frequently. The frequency of the atrioventricular node is 45 beats per minute, which will guide the heart when the previous one fails. If this also fails, the ventricles can work with a frequency of 20-40 pulses per minute. These frequencies, however, can be too small, especially in situations where the body needs great needs, such as effort. The main symptoms of this dysfunction may be fatigue, respiratory failure, dizziness or loss of consciousness.
Through the electrocardiogram we can know where the stimulus occurs and how it spreads. The most common pathology is the blockage of the stimulus in the atrioventricular node, so the atria contract 70 times per minute, but the ventricles only 20-40 times.
For the ventricles to go faster, it is enough to take a cable there, connect a battery and stimulate as often as we see fit. This, however, affects coordination between atria and ventricles: blood does not pass well enough from the atrium to the ventricle and these do not pump enough blood. To avoid this problem, in those cases where it is considered appropriate, two cables can be placed, one directed to the atrium and the other to the ventricle: the atrial cable will generate the same excitation that is given physiologically, and a little later, the ventricular will excite the ventricle synchronously.
The wires currently used, in addition to their excitation capacity, have the possibility of “listening” to what happens in the heart. What would happen, for example, if the atria contracted correctly but the impulse did not reach the ventricles due to the blockage of the atrioventricular node? The atrial cable would hear the function and soon after the ventricular would lengthen the impulse. The advantages that this implies are immediately understood. Our heart does not always go with the same frequency: while we sleep, slowly and effortlessly. The pacemaker does not find it easy to distinguish these rhythms, when and when they are slow, so the atrium works normally is a perfect reference. However, although less perfect, taking as a reference the movement of the body or other parameters, it has managed to create a pacemaker that can vary its frequency.
Apparatus with local anesthesia
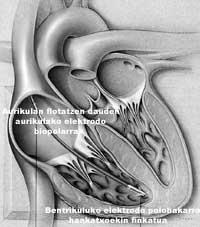
Although in emergencies the cable is placed and the provisional battery is left out (called an external pacemaker), when the patient's needs are well studied and the final device must be placed, it must be operated, but it is not a complicated operation.
A chest vein is placed and the cable is passed into the right atrium, ventricular, or both. When x-ray or other control systems check that the cable or cables are well located, the battery is placed. Around the perforated vein a small wound opens and under the skin a bag of the size of the pile opens. Connect the battery and cable and sew the bag. A couple of days home. Well, that also has its risks, it is not always so simple, and these problems can become serious in some cases.
Once the pacemaker is installed, reviews will be made. The first is that before the patient leaves the hospital, the cable has not moved and everything is fine. Then once a month or, depending on the patient and the center. On the pile, placing a device on the skin, we can know its state. In addition, we can modify eleven parameters (frequency, stimulus power, rhythm regulation orders, etc.) as circuits and computing advance, more and more.
Batteries last approximately ten years. When it runs out, open the wound, remove the old one and place the new one. It is also necessary to check the condition of the cable as it can deteriorate or break over time. In these cases the process is somewhat more complicated as it is necessary to place a new cable.
Pacemakers are used to treat slow heart rhythms, but they can also play in cases of fast rhythms. They may also serve to treat some death causing arrhythmias, for example, but we will leave this for another article.
To keep in mind

Interference between pacemakers and some devices is known. Although most of them have sufficient protection, care must be taken with microwaves, high-voltage lines, electric deburring machines, electric toothbrushes or similar appliances. Attention should also be paid to magnetic fields such as resonance.
You know, reader: if you don't need it, better. If you need it, however, you can make a totally normal life with the pacemaker, even in stress conditions.





