Food and mental health, confused relationship
In recent times, numerous studies are being conducted to clarify the relationship between food and mental health. Many studies show, for example, that there is a direct relationship between consumption of ultra-processed foods and the risk of depression. However, the factors, mechanisms and consequences of this relationship are not well known. Researchers try to answer questions for their usefulness in prevention and treatment.
It doesn't take a long time to find a study that looks at the relationship between ultra-processed foods and depression. In a study led by the University of Navarra, for example, almost 15,000 students from Spanish universities were followed for 10 years. Initially, they did not have depression, but of them, 774 were diagnosed with depression in this interval and, of the analyzed variables, concluded that the tendency to consume ultra-processed foods increases the risk of depression.
This study was published in the European Journal of Nutrition in 2019. Since then, research in other countries and in other population groups has reached similar conclusions. For example, in the United States, a study conducted by Harvard University investigated more than 31,000 women between 2003 and 2017. In this research, at first none of the participants had depression, and the objective was to clarify whether there is a relationship between consumption of ultra-processed food and the development of depression.
The results were published last year in the journal JAMA Network Open, and confirmed this relationship, as well as the influence of other factors related to depression such as age, food calories, body mass index, fitness, tobacco and alcohol consumption, comorbidities (diabetes, hypertension, dyslipidemia), income, social relationships, bellota state. They also looked at the ingredients in ultra-processed foods and found that the risk of depression is mainly related to artificial sweeteners.
In the other sense
Considering that the relationship between diet and depression is bidirectional, inverse analysis studies have also been performed, that is, whether healthy eating is effective against depression. A study published last November analyzed, for example, the influence of the Mediterranean diet. Specifically, they wanted to know if the Mediterranean diet and the consumption of olive oil serve to prevent residual symptoms and redepressure. Participants were men and women aged 18 to 86 years who had suffered at least one depressive episode in the last 5 years and who had overcome it totally or partially in the last 6 months. The result was encouraging: participants who followed this diet were less likely to have residual symptoms and develop depression than those who followed a regular diet.
This research was carried out under the direction of psychiatrist Beatriz Cabrera Suárez, of the hospital of Las Palmas (Gran Canaria), with researchers and participants from Navarra and Álava. In 2022, Cabrera presented his thesis entitled: “Mediterranean diet and prevention of recurrent depression”. In his thesis he studied, among other aspects, the influence of the components of the Mediterranean diet on depression, as well as the pathophysiological aspects of depression and, within everything, the relationship between inflammation, intestinal microbiosis and depression.
Gut-Brain Axis
In fact, according to Cabrera, “physical and psychological stressors can alter the composition and metabolic activities of the intestinal microbe, increasing the inflammatory (Clostridium, Streptococcus, Klebsiella and Acterlibacter, for example) and decreasing those of other anti-inflammatory (Lactobacis, Llubifidobecium and Acterias). More Bacteroidetes and less Lachnospiraceae have also been found in the feces of people with depression.”
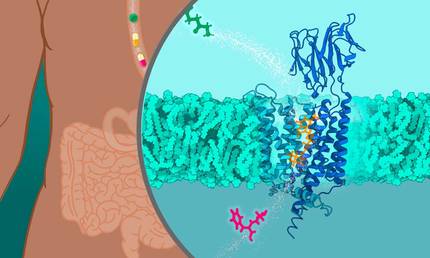
In addition, Cabrera has pointed out that signals produced by the intestinal microbiota can affect the brain and emotional responses. And it also raises the hypothesis of a depression mechanism. According to him, “microbial disorders increase the risk of depression as they cause a chronic inflammatory state that affects the mood”. Proof of this are IgA and IgM immunoglobulins in plasma against the lipopolysaccharide of Enterobacteriaceae bacteria in depressive patients.
A CSIC research group has also patented a bacterium that can be useful in treating depression, based on the possible association of microbial disorder with depression: Chistensenella minuta. This group is led by pharmaceutical researcher Yolanda Sanz Herranz, who assured that in the first trials he was a good producer of serotonin in vitro: “It was an interesting discovery, as the concentration of this neurotransmitter is decreased in people with depression and stress and plays a fundamental role in emotional regulation.”
Subsequently, it was tested in vivo in animal models depressive for chronic social stress and demonstrated that, in addition to promoting serotonin production, it reduces the excess corticosteroids that produce stress. Therefore, the results were considered encouraging. In fact, according to researchers, two-way communication between the intestine and the brain is based on endocrine, immune, and neural networks, and it works as a channel for reporting organ functions and health status.

“If we gain a deep understanding of the communication processes between the intestine and the central nervous system, we will understand the reactions that occur in the body in traumatic or dysfunctional situations and we will be able to work precisely on certain problems,” says Sanz.
Egg and hen
However, more research, better knowledge and more evidence are still needed to use certain diets or intestinal microorganisms to treat depression. “Food helps treat psychological disorders, but it’s not enough and there are no miracle recipes,” Elikaeskola’s experts warn.
Elikaeskola's team consists of dietitians, nutritionists and psychologists, under the direction of Eli Gallego Moreiro. They are specialized in the treatment of gastrointestinal diseases and eating disorders. It is not unusual for the patient to present signs of depression. And from the beginning Galician has made clear: “There’s a lot of talk about the connection between the gut and the brain, and some even consider the gut as the second brain, but there’s a lot of misunderstanding there. When they say the happy gut brings a happy brain, it's not true."
He explains that functional digestive disorders now change their names and are technically called gut-brain interactions. “Although the name can reinforce false convictions, it has nothing to do with this question of the happy intestine. It is important to be clear that it is not in our hands to be depressed or not. And sometimes they make patients believe that with a given diet they will overcome depression. This puts all the responsibility on the patients and, if they cannot strictly follow the diet they have been given, they suffer very badly. This, besides not being true, is absolutely unfair and harmful.”

Gállego has also given examples: very expensive diets, with ingredients that are difficult to obtain… “They are not general, but we see them a lot. Many don't have the money to do the diet they've been given, and then they take away the most expensive foods and stick to a very poor diet.
In addition, therapists sell components made in their lab, which of course are not cheap. All of this is detrimental to patients, since, physically, it increases dysbiosis or bacterial imbalance, and also psychologically because they feel they are not able to fulfill the promises. We know many such cases, and I tell everyone that, for treatment to succeed, they will need psychological support. On the other hand, we show that physical exercise has a beneficial effect on depression, but eating has a very limited effect.”
When talking about studies that analyze the relationship between depression and food, they have also taken the word Jone Larrañaga Zumeta, a colleague of Gallego, and Garazi Lizarraga Lertxundi, who have agreed that “what is anterior, egg or hen”. That is, to what extent inadequate feeding is the cause or effect of depression. Larrañaga clearly said: “If you’re not well, you’ll find it hard and hard to organize meals, choose the food that suits you, buy, cook… In addition, it’s true that ultra-processed foods have the ability to produce pleasure neurotransmitters, like dopamine.”
In this sense, Gallego has reminded us that we tend to link food with emotions caused by education and culture: “We associate parties and celebrations with certain meals and obligations to others. It’s very rare to put broccoli on a party menu.” This aspect is also discussed at the School of Food.

Regarding treatments based on certain microorganisms, Gallego considers that “converting data into projectiles”. “When a study says that everything is solved with a probiotic, it’s not. There are a lot of research, but very few have been done in people and you have to see what other variables there are. The studies are very heterogeneous, and drawing from one of them general conclusions is by no means correct.”
Personalized treatment
Within this mix, members of the School of Food alert about the risk of treatments without scientific basis: “We have had patients who have performed a colon cleanse, on medical recommendation, in presumably qualified centers. What they're selling is that they have depression or anxiety from the effect of the microbe, or whatever, and to cure it first, they have to clean the gut microbiota. But the result is often unfortunate. There may be some cases, such as an infection of the bacterium Clostridium difficile, in which you have to do it, that is, first clean the microbiota and then raise the new one. But, if not, these extreme treatments can be very harmful.”

In particular, Lizarraga has underlined the need for each patient to be specifically analyzed and treated in a personalized manner. “It is true that it is often frustrating for patients to hear that the therapeutic process will be slow, need help and that there are no wonderful pills.” “It must be clear that these are long processes, that they will occasionally relapse, and that the diet is important but not enough,” adds Gallego.
The members of the Food School have therefore recommended that simple precautions be taken: “Until we know better the relationship between the brain and food and know how to use this knowledge in prevention and therapy, we should be careful with these types of messages.” Meanwhile, they will continue to investigate and learn.






