Hepatitis B
It is a disease that passes from one person to another through a virus, although it is spread throughout the world, it has a different incidence from one country to another. It is important to have a high incidence, but it is still more important to note that between 5% and 10% of patients will evolve into a chronic disease. In short, it is these chronic diseases that maintain and greatly expand the disease. In addition, we must not forget that 40% of chronic patients who reach maturity will die from disease: chronic liver disease, cirrhosis or carcinoma of the hepatic cell.
Currently, this disease has no effective treatment and can only be controlled by preventive measures at the community level. In recent years, the etiological agents of this disease have been fully known, developing effective measures to eradicate the disease. One of these measures is that of txertuga. The breakdown of the epidemiological chain of the hepatitis B virus through cheru.
Epidemiology of Hepatitis B
Hepatitis B virus is Hepadnabirus (DNA virus), with penetration capacity in the liver cell and can cause hepatitis.
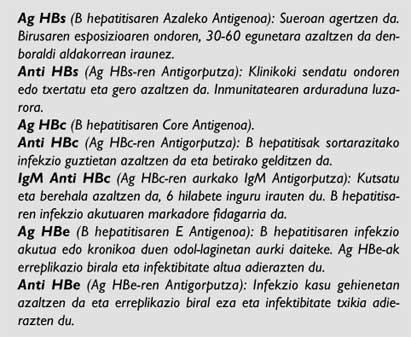
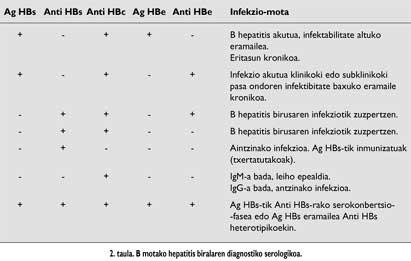
This virus is joined by several Antigens (Ag) and Antibodies (Ac) (Table 1). The explanations of these antigens and antibodies in the body of people help to know the current state of health (acute disease, carrier...).
For this human virus, no reservation animals or vectors are known. The actual reservoir of this disease is a contaminated person, that is, a person in incubation age, in acute phase of the disease or in a situation of chronic carrier. Age or sex is not important in the transmission of the disease.
This disease is mainly transmitted by contact with the blood of infected people or with other body fluids. The risk is for anyone, but especially for those who put themselves in danger of this contact still have more. Thus, sexual relations, the injection of venous drugs, the transmission by birth (mother to child) can be some of the best known ways to spread this disease.
Means of transmission
Hepatitis B virus infection can pass from one person to another through another liquid contaminated with blood or body.
Among the transmission routes stand out:
- Heterosexual and homosexual relationships.
- Venous injection of drugs.
- Transmission to birth (mother to child).
- Blood transfusions. Currently the risk of contamination by this route is very low. This is because all donors are seen whether they have PCI or not and a selection is made before they are donors.
However, a percentage of patients with hepatitis B are not identified with any risk factor.
Carrier Hepatitis B
Hepatitis B virus infection can be asymptomatic (in more than 50% of cases) or symptomatic. A person with acute hepatitis B infection, with or without symptoms, can become a chronic carrier of the disease.
To identify a person as a chronic carrier, blood tests performed on at least two occasions (keeping a period of six months) must provide Ag HBs (+) or Ag HBs (+) and IgM Anti HBc (-) a single analytical. (Table 2)
Although the connectivity of carriers is related to the positivity of HB Ag, provided that this carrier can potentially contaminate another.
The likelihood of a person becoming a chronic carrier is greater if he or she has a disease in the first years of life. Thus, if the disease is suffering in newborn children it is likely to become chronic carriers in 90-95% of cases, if they are younger than 5 years in 25-50% in cases and in adults in 6-10%. However, immunosuppressed people have a higher risk of disease forever.
In many chronic carriers no clinical signs appear, but in the long term these people have a higher risk of liver cirrhosis or cancer. Especially those within this group are those who largely transmit the disease, so the carrier must always be considered as a person who can spread it to another person.
Vaccination against hepatitis B in Nafarroa Garaia
The most effective measure against hepatitis B is vaccination. For this reason, in Nafarroa Garaia, since 1993, newborn children and students of 7th Primary Education are offered vaccination against hepatitis B.
The first dose is given to newborn children before leaving the Hospital, in most cases on the fourth day after birth. The second and third doses are placed in the Health Center corresponding to each area.
To students of 7th E.G.B. They are placed again in the corresponding center.
In addition to the two groups cited and from 1994, other characters are also invited to participate in Hepatitis B. Vaccination will be recommended especially to people at high risk or in the following cases:
- When the profession is a way of risk. Among others, health personnel (for the risk of bleeding substances).
- People with intellectual disabilities in organizations and their caregivers.
- Hemodialysis. It is always convenient to perform the vaccination before proceeding to the hemodialization.
- Recipients of body transplants and blood products. It is recommended that people who have carried out blood transfusions perform a pre-vaccine test.
- People living with chronic carriers and sexual partners of hepatitis B virus carriers. These people will be made a previous marker and will be inserted later (to which they are susceptible).
- People who take drugs by venous means and live with them. These also have to make markers before inserting them. However, vaccination is also possible if the drug has begun to be used recently. Once the 3 doses of Txeritu are taken, you will have to see the levels of Anti HBs, especially in the case of HIV (+).
- Sex with different people (who have had more than one sexual partner in the last 6 months).
- Persons in prison.
- Infection of viral hepatitis B from endemic countries.
- International passengers. If you are going to spend more than six months in areas with a high infection rate. Or in the case that due to the performance of its activity in the Health Center or in the Hospital there is a risk of contact with the blood for a short period.
- Members of the community of high endemia, such as gypsies.
Access to access Access
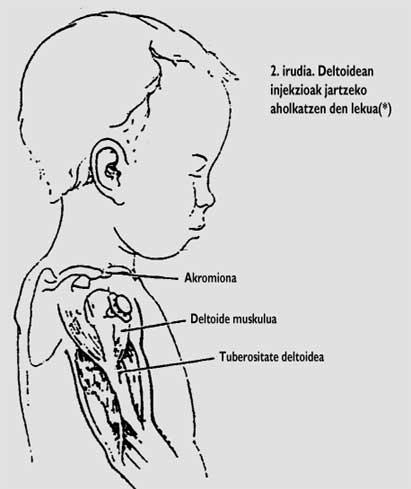
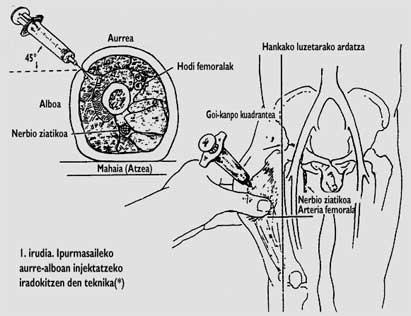
Intramuscular injection of the kid against hepatitis B. Children and adults are placed in the deltoid muscle and newborns in the muscle of the prefix of the ear. It seems that adults are reduced to immunogenicity by placing them in the buttock, since in many cases it is replaced by adipose tissue instead of placing them in the muscle.
Model of insertion
Children and adults are injected into three injections. The second and six months after the first dose (0, 1 and 6 months).
The recommended doses will be different. This should take into account the product or age of the recipient or status of the mother's Ag HBs in newborns. Hemodialized and immunosuppressed, for example, more or more doses are advised.
If Chuso against Hepatitis B is combined with other cavities, it has so far produced no interference in the manufacture of antibodies.
If, for any reason, vaccination ceases after the first dose, the second dose will be put as quickly as possible. Therefore, between the second and third doses, a minimum period of two months must be maintained. If the dose that is delayed is the third, it will be reset when appropriate.
This affection against hepatitis B does not cause any related damage. However, among children and adults who have contracted the pimple some side effects have been described, so in some cases (between 3 and 29%) the injection site is usually pain or to a lesser extent (between 1 and 6%) the fever is higher than 37.7 °C.
Insert Markers Insert Markers
After insertion, in some cases it is recommended to perform markers such as: Positive HBs for newborn mothers, dialysis patients, waiting drug receptors, HIV(+) and chronic carrier couples.
These markers must be made between a month and six months after insertion. In this analysis, it is recommended that Anti-HBs are less than 10 IU/L.