From donation to blood production

The blood is golden for our body, essential for its proper functioning. At first glance it only looks like a bright red liquid. But the color is not the only one that is intense, since the blood is a living tissue.
The microscope is very useful to know the secret of this wonderful liquid, as it highlights different types of cells found inside the blood: red blood cells, white blood cells, platelets... Blood has many other components that make blood very important in the functioning of the body. Without blood you cannot live!
But for those who began to transfuse blood from one body to another, blood hid these and more secrets. For example, they did not know where the blood was circulating, nor what to say has that functions fulfilled the blood.
Blood transfusions underway

It seems that the first blood transfusions were performed from one animal to another. With a syringe they took a few drops of blood from a dog and put them in another dog, for example. Then, from the animal to the human being they transfuse. They acted to heal the sick, but with bad results.
The first blood transfusion to a human being was performed in 1667 by the doctor of Louis XIV, Jean-Baptiste Denis. He brought blood from lamb to a very sick young man. Other authors of the first transfusion were the English Lower.
Since then, the disputes between France and Britain were endless in terms of blood transfusion, so both wanted to impose themselves. But the debate was losing strength, as blood transfusions did not have the expected success. Failures of this type of therapy were initially attributed to poor health of patients. But in the end, both in France and England limited the use of blood transfusions and was banned by the Pope of Rome.

Many years went by until blood transfusions regained strength. XIX. In the 20th century a few doctors resumed their work with transfusions. By then they did not use a simple syringe, adapted the utensils and passed the blood from one man to another.
Birth of hematology
However, there were many recipients who responded badly to the blood received. When blood plasma began to separate from other components, they discovered that something caused not all blood to be compatible. Today it seems evident, but at that time the concept of compatibility or blood groups was not known.
When the blood of two people is mixed, in some cases red blood cells clump together. This can be seen at first glance, as coacids are formed. This reaction was the cause of the failure of many blood transfusions. Well, the Austrian doctor Karl Landsteiner wanted to investigate this reaction in depth, extracting blood to his colleagues in the laboratory to check the compatibility between them. It dates from 1901.

Landsteiner separated the serum from the blood, the blood plasma, from the red blood cell, and then mixed each serum with the red blood cells of the remaining samples, one by one, to see if an agglutination reaction was occurring. Completing a table with the results, he distinguished three types of red blood cells: A, B and O. Thus arises the concept of well-known blood groups. Group AB split two years after the rest.
No wonder the AB blood group does not appear in the initial session, as it is quite rare. Only 4.5% of the European population has AB blood. It is therefore understandable that this group of blood appears in any of the samples taken by Landsteiner.
Separation of blood groups was a breakthrough, but there are also more factors that influence compatibility. The Rh factor, for example, was discovered in 1940 by Landsteiner himself accompanied by Alexander Salomon Wiener. By then it was known that the superficial antigens of red blood cells were those who knew the antibodies of the blood plasma of the receptor and favored the immune response.
Compatibility keys

Red blood cells can contain many different antigens. When talking about the Rh factor, for example, it is not the only antigen. Although blood is classified as Rh positive and Rh negative, this factor actually depends on the combination of six antigens. These antigens are D, d, C, c, E and e. But antigen D is the one that causes in all of them the most violent reaction of antibodies, so it is generalized: Rh-positive is said to have D-antigen and Rh-negative ones that do not have D-antigen.
However, the ABO system is undoubtedly the most well-known blood classification system. This system is classified according to type A and type B antigens. Those in the blood group A have antigen A, those in the B antigen B, those in the AB and those in the blood group A and B and O have no antigens of this type in the red blood cells.
The blood compatibility of the different blood groups depends on these antigens, since the antigen A has no plasma antibodies that react against A, but yes against B, while the blood containing antigen B contains antibodies against antigens A.

The AB blood does not contain antibodies against antigens A and B, so the AB blood receptor may receive blood from any blood group. Instead, in the blood of group O there are antibodies against A and B, so the receptor cannot receive blood that does not belong to the same group.
Rh is a special antibody system, since antibodies to the Rh system, like antibodies to the ABO system, are not proper, but occur when the antibodies come into contact with the blood containing the antigens of the Rh system. That is, a person with Rh-negative blood does not have antibodies to Rh-positive blood, but it is enough that once contact occurs antibody, for example during pregnancy or by a blood transfusion.
However, as already indicated, there are as many antigens that produce agglutination reactions, although the most violent occur when an inadequate ABO blood group is transfused. According to these antigens there are numerous separation systems of blood groups: From Lewis, Kell, Kidd, Duffy...
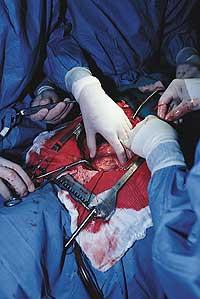
At present there is great care in the realization of a blood transfusion, and in addition to using the blood of the group and Rh corresponding to each receptor, previously the compatibility of both blood is checked by a cross test, that is, the blood of the recipient and the donor is mixed on a plate to check if an agglutination occurs.
Blood in War

The problem of blood compatibility is well above. But there is another problem that comes from a long time ago: the persistence of blood. When World War I broke out, it was known that there was nothing like blood transfusions to treat injuries that had lost a lot of blood, but in order to use it in the war, blood had to stay longer.
At that time, research to preserve blood advanced greatly. On the one hand, the addition of sodium citrate prevented coagulation and, on the other hand, the use of refrigerators allowed blood to reach combat zones. During World War II blood transfusions were considerably extended and it is said that 380,000 blood units were used. In 1982 British soldiers received blood on their trip to Malvinas, which allowed them to freeze that blood and transfuse the wounded.
Currently the blood lasts 35 days, of course, treated correctly. Over time proteins are denatured and hemolysis occurs. However, this expiration period has been extended for special situations such as wars.

But in 1982 there was a problem that worried society more about blood transfusions: AIDS. Although the details of this disease had not yet been clarified, it was constantly spreading. And as was later known, one of the ways of spreading the virus was blood transfusions. The insecurity of transfusions triggered the alarm and decreased the number of blood donors that had been growing up until then.
It was a great setback for blood transfusions. The blood that until then was a source of energy and health became dangerous. People saw transfusions with suspicion and feared anything related to blood.
However, by 1986 measures were taken and the order was established to analyze all donated blood. However, the number of donors increased again. In fact, blood donation was established as a voluntary act, could not force anyone to donate blood and was an altruistic act.
Thanks to voluntary donation action, blood is obtained for free, but do not believe that blood is cheap. It has been mentioned that for the body is urregorri, but also for the pattern of the health system. If you take into account the value of the blood bag and the analytical tests that are done to ensure that that blood is safe, each blood bag or blood unit has a minimum value of almost one hundred euros.
In search of the perfect blood
Therefore, blood is expensive, it should last longer and sometimes runs the risk of transmitting diseases. Therefore, one of the strengths of researchers today is to get cheaper, much longer and totally safe blood.

Anyone who gets a synthetic or artificial blood that meets all these characteristics will have a poplar. So far synthetic blood has been obtained, but not as artificial as its name suggests. In fact, among other things, it has been achieved through the transformation of ‘natural’ blood; the treatment of human blood allows the obtaining of blood without antigens or pollutants, thus obtaining a universal blood that serves the receptors of all blood groups.
The problem with that blood is that it does not meet the third condition of being cheap. But it is very useful for war, since transfusion can be performed without having to perform a cross test, that is, you do not waste time knowing the blood group. Somehow, it is universal blood.
To get a cheaper blood you can use the blood of animals. Pig and cow blood are some of the tools used for research. But this path has another difficulty: make sure that no disease passes from the animal to the human being.
However, in transfusions blood is rarely used entirely, normally its components are separated: red blood cells on the one hand, white blood cells on the other, platelets and blood plasma. Therefore, the collection of these components by synthetic means is also studied. Good results have been achieved with red blood cells and plasma, but not with white blood cells and platelets.
Red blood cell transfusions are done in severe cases of anemia and in cases of injuries that have lost a lot of blood. In these cases, the muscles receive little oxygen. And because oxygen is transported by the hemoglobin of red blood cells, the laboratory looks for synthetic hemoglobins that can carry even more oxygen. For example, using fluorinated materials or replacing the iron atom in the core of hemoglobin with another metal.

One of these synthetic hemoglobin substitutes, Polyheme, has provoked great conflict in the United States. This compound has begun to be tested in ambulances. The controversy arises because the patient has no decision-making capacity at the time, as it is used in case of serious injuries.
However, the success of Polyhem is a revolution in emergency services. But laboratories that are developing other products are not asleep, do not want to stay behind and want to get their ‘synthetic blood’ as soon as possible.
Some components of blood plasma can be synthesized today, such as factor VIII for hemophiliacs. Many compounds are obtained from blood plasma such as vaccines, gammaglobulins, factor VIII... For the industrial production of these substances it is necessary to allocate large amounts of plasma from blood donors to the industry. Synthesis in the laboratory facilitates the process.
It is observed that real artificial blood is still far away. In fact, it is not possible for the time being to synthesize red blood cells, let alone platelets and white blood cells. Only artificial substitutes of a few blood components have been obtained. And, for now, the only one able to synthesize blood is the human body. However, progress is constant and, before you can imagine, we will have a synthetic blood substitute.
A treasure full of secrets
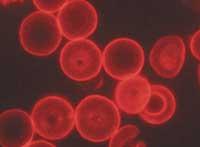
The researchers performed the first transfusions that would hardly imagine the complexity of the blood. Thus, a square centimeter of blood contains between 4.5 and 5.5 million red blood cells or erythrocytes, between 7 and 12 thousand white blood cells or leukocytes and between 150 and 400 thousand platelets; and, in blood plasma there are hormones, mineral salts, vitamins, proteins and other compounds.
All these components are necessary for the proper functioning of the body. Blood is an effective vehicle of food and waste. It also performs eleven functions, including mechanisms to prevent bleeding and protect the body from infections.
Opportunities, the best of oneself
For a transfusion, the compatibility of blood groups is taken into account, but blood from the same blood group as the receptor is preferably selected. That is, when the recipient can receive blood from another group of blood, the first option is blood from the same group.
For example, those who have blood from the AB group may catch blood from any other group, but the first option is to enter blood from the AB group, if it is not possible to use the blood from the A or B group and the last option is the blood from the O group.
In some emergency cases, especially when there is no time to know the patient's blood group, blood from group O, a universal donor, is used. However, in these cases blood for transfusion usually does not have plasma, avoiding antibody reactions in blood of group O.
With the Rh factor the same is done. Rh positive blood may take Rh negative, but the first option is to introduce Rh positive.
However, before transfusion, the laboratory ensures blood compatibility by contacting both blood.
However, when possible, autologous transfusions are performed, that is, your blood is introduced to the patient. A few months before a previously scheduled operation, the patient donates blood, avoiding many possible risks, since the immune system will hardly fight the blood itself.
The way of blood

Donor blood travels a long but fast path until it is received by the recipient. In each performance a unit of blood (450 ml) is collected in a special bag that is taken to the blood bank. Blood donation also collects small samples for conducting analytical tests that ensure the absence of potentially dangerous diseases for the recipient, including HIV testing and hepatitis B and C testing.
Most of the blood that reaches the blood bank is distributed into components. Units of red blood cells, platelets, and plasma are prepared. However, approximately 90% of plasma is destined to the industry for albumin, gammaglobulin or compounds such as factor VIII. These compounds are used to treat many diseases.





