Medical effects of nuclear accidents. 5th anniversary accident Chernobil


On April 26, 1986, the largest nuclear accident in the world took place in the Chernobil of the Soviet Union. Given that this year is 5 years old, it seems appropriate to talk about the consequences of this accident and, incidentally, any nuclear accident. Since the subject is too broad and our specialty is Hematology, we will focus mainly on the hematological consequences. However, we cannot fail to mention many other details, starting with the most urgent measures after the accident and ending the long-term consequences.
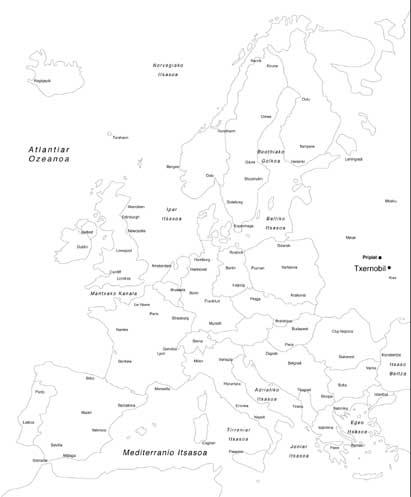
In the Chernobil accident, a 50 mCi radiation and the same amount as noble gas were released. 25% was released immediately and the rest in 10 days. After the terrible explosion of the reactor, a radioactive fog that was initially directed to the northeast was launched 10 km high. Before 36 hours of the accident 45,000 people were evacuated from the town of Pripiat, located 2-4 km from the reactor. During the next 2 weeks approximately 90,000 people were evacuated from the zone 30 km from the central one.
In this accident it was possible to verify that the immediate evacuation is not always adequate. In the case of Pripiat, it was delayed until getting the necessary buses and choosing the right tracks that were not affected by radioactive fog. In addition, a polymer layer was removed to reduce the inhalation of radioactive dust on the earth's surface. These measures had positive consequences, since the population of Pripiate had taken less radiation than many people who lived farther away. However, the evacuation plans must adapt to each situation and, if not, think about how things would change if the radioactive fog had skyrocketed and the wind had sent it to Pripiat.
Effects of radiation on people
Depending on the type of radiation, ingested doses, administration time, full body, etc. According to the World Health Organization (WHO), the effects according to the dose received would be:
- More than 2 Gy: it will affect the bone marrow, that is, the area of blood production, so for 2-4 weeks will appear the decline of the blood cells (pantzitopenia) and the destruction of the defenses of the body (immunosuppression), resulting in a risk of bleeding and infections.
- 5 Gy: supporting with antibiotics and transfusions, 50% of people are doses of death.
- 7 Gy: 90% of people are doses of death.
- More than 10-12 Gy: apart from the effects of the blood appears gastrointestinal toxicity, occurs the fall of the epithelium of the intestinal mucosa, the appearance of diarrhea and infections and the death of 6-9 days. Other organs also have effects.
- More than 50 Gy: they will die a few days for neurotoxicity and cardiovascular failure. In addition, redness and hair loss will appear on the skin first and then peeling and wounds between folds.
Finally, it must be taken into account that explosions and consequences of fire can appear in nuclear accidents.
Measurement of the dose received
There are two measuring pathways:
- Physical Environmental monitors can be used, but in Chernobil most were destroyed or could not be recovered. We also have individual dosimeters, but they were not prepared for these irradiation levels and were destroyed or lost due to the characteristics of the accident. In the future they can be improved with the remote control of the environmental monitors and with special meters for accidents.
- Biological Before we have commented that radiations provoke pantzitopenia, that is, we can know the dose of radiation obtained by analyzing the decrease of the blood cells and the days in which we decrease. To complete the data, we can analyze the changes that appear on the chromosomes of the blood cells and bone marrow.
Immediate medical measures after nuclear accident
The decision and fate of the evacuation after the accident remains in the hands of political institutions.
Let's say what the International Commission against Radiation advises: In integrated doses less than 0,25 Gy the evacuation is not necessary, it is necessary from 0,75 Gy and in doses less than 0,5 Gy will be analyzed the risks of evacuation, the precision of the estimation of dose, etc. before making decisions.
The radiated persons will move as soon as possible to the hospitals enabled for it. The contaminated garments will be removed, the skin will be cleaned and decontaminated, eliminating all the dirt that may have on the wounds. If radioactive substances have been ingested, give vomiting excrement or laxatives. The most frequent radionuclide in this type of accident is I 131. I 131 is widely used in hospitals and has not increased the frequency of thyroid cancer. All this without prejudice to the fact that I 131 does not imply carcinogenic risk.
If I 131 is ingested by mouth and inhalation, it will concentrate on the thyroid gland before an hour. There is a substance that blocks the concentration of I 131 in the thyroid gland if taken before I 131: potassium iodide.

The problem is that: If I is taken after 131, if within 6 hours the loss of the blocking effect is not taken, it is useless to take potassium iodide later. Therefore, their effectiveness in nuclear accidents should be dealt quickly and people should know when and how to take them.
Its use would generate many problems for public health: knowing that it prevents certain thyroid cancers, its economic cost is high, its distribution would generate great problems, it is very difficult to know how people have taken it in such a short term, etc. On the other hand, we must know that it can produce side effects and that people should know how to protect us from all radiations, only from I 131. Probably in most nuclear accidents the results would be low. In Chernobil it was distributed a few days around the nuclear power plant and time will tell if the results have been satisfactory.
In most cases, gastrointestinal symptoms and changes in the blood will be taken into account to determine the person who should be sent to the hospitals, that is, the Acute Irradiance Syndrome. The main symptoms are anorexia and tambres, and the higher the acquired radiation, the earlier they appear. The basic thing is to perform a blood test (hemogram) to all people who receive radiation and repeat it at 3 days.
Treatment of hospitalized patients
Once the skin is clean and decontaminated, similar topical measures will be taken as usual in burns and grafts will be made when necessary. The serums will be essential for the treatment of gastrointestinal syndrome and, being unable to ingest almost anything orally, the feeding given from the vein will be applied. Unfortunately, few seriously affected patients will come out alive because hemorrhages and infections will push them to death.
As mentioned above, the pantzitopenia (decrease in red blood cells, white blood cells or leukocytes and platelets) will be explained in the blood, so we should keep them with transfusions.
They will need transfusions of the platelets needed mainly for blood clotting. Decreased need for transfusions of hematies or red blood cells for longer life. Sometimes, when the gastrointestinal lesion is high, they will also need plasma.
The reduction of leukocytes considerably increases the risk of infection and if possible they will be kept in isolated rooms.
Bone marrow transplant
When you want to perform a bone marrow transplant in leukemias and other hematological cancers, the patient is radiated throughout the body, giving 12-16 Gy. As a result of radiation, the diseased bone marrow is destroyed and the bone marrow of a donor is subsequently transplanted to make blood.
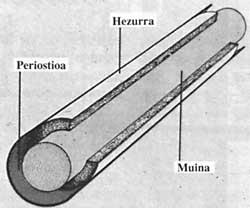
We keep the patient with transfusions until the new bone marrow can produce enough blood. Something similar can be done after nuclear accidents, but deciding which patient will be transplanted is not easy and the following points should be taken into account:
- Complications derived from bone marrow transplants will be 30%.
- The transplant may be performed to people who may die from the failure of the bone marrow as a result of radiation, but making sure that the lesions that suffer in other places or body viscera will not die; otherwise, the transplant would be useless.
- Compatible donors will only find one in three.
- We must take into account the age, since in older than 45 years the bone marrow transplant has an excessive mortality.
- To the complications derived from bone marrow transplantation, we must add those produced by radiations in other viscera.
Before the accident in Chernobil, two bone marrow transplants have been performed in nuclear accidents. In 1858, an incompatible bone marrow transplant was performed for 5 people in Vinca (Yugoslavia) and 4 survived. However, the dose of radiation received is unknown, and if the transplant has been adhered. For the second time, in 1867 it was held in Pittsburg, where a person was made a transplant of his twin brother and left alive, but being twins we do not know if his new bone marrow is proper or twin.
With the suspicion of the Chernobil Acute Radiation Syndrome, 202 people were transferred to the Radiology and Hematology Services of the Moscow Clinical Hospital 6.
Of these 105 received a radiation of 1-2 Gy. Another 33, due to their greater radiation of 6 Gy, were suitable for bone marrow transplantation. However, only 13 people were transplanted from bone marrow for different reasons at 7 days (4-16) after the accident occurred. The mean age of 13 receptors was 27 years (23-46) and 12 had burns. In this work we cannot mention too many details, but we must say that 13 died 11. Two patients survived with burns and cataracts. In these two cases, the transplanted bone marrow was pasted, although its bone marrow was later regenerated and the transplant was overcome.
It is clear, therefore, that after nuclear accidents, bone marrow transplantation has a limited value. However, we can recommend bone marrow transplantation for people with radiation greater than 8 Gy.
Stimulating factors of bone marrow
Currently, significant advances are being made in the use of factors that accelerate the formation of bone marrow cells, which could require their use in radiation doses of 5-8 Gy. In these doses there would still be a cell capable of producing blood in the bone marrow and if there were stimulating factors it would produce blood cells before, decreasing the risk of complications.

On September 13, 1997, two people discovered in a closed clinic a capsule with radioactive isotope Cs 137
What happened was known on the twentieth of September, but by then 249 people had radiated. The situation was as follows: They were easily decontaminated 129 because they only had light contamination in clothes and skin, 79 were followed in external consultations by deeper skin contamination, another 50 received a higher dose of radiation and were taken to 20 hospitals. They were taken to 10 Rio de Janeiro, with bone marrow defeat. In 8 cases, a stimulant factor was used, which accelerated the production of granulocytes and macrophages. Granulocytes and macrophages are a type of leukocytes and white blood cells that defend us against infections. Of these 8 patients, 4 survived and another 4 died, since at the time of starting treatment they were infected.
At present, great advances are being made in the research of stimulating factors. For example, a factor has been synthesized that accelerates the production of platelets necessary for blood clotting.
Long-term effects of radiation
We can divide these conclusions into two groups:
- Produced in somatic cells.
The radiations will appear in the person received and can be of two types:
- Nonstochastic calls: The effects are dependent on doses and occur in all people who receive the same dose. Hypothyroidism, cataracts, delay in growth and sterility belong to this class.
- So-called stochastic: only some people will develop pathology after radiation without the planned options. In this group we can include cancer, teratogenic effects (pathology explained in the children of pregnant women of the time, especially mental retardation) and genetic effects.
- Produced in germinal cells.
The pathology is manifested in children.
In the effects of short-term radiation, the problems that I 131 can cause in the thyroid gland have been mentioned. When hypothyroidism, i.e., supposes a functional restriction of the thyroid, you will probably have to take thyroid hormones throughout your life. On the other hand, time will tell whether radiated people increase the frequency of thyroid cancer.
Radiation increases the frequency of other cancers, as has been observed after atomic explosions. The most common cancer is leukemia, with a risk ranging from 3-5 years to 5-10 years. Other hematological cancers, such as myeloma, also appear. Solid cancers, such as lung, breast, and bone, will also appear more often. The highest risk occurs at 10 years of age and continues at 20-30.
As a reflection
Given the severity of the accident in Chernobil, more people could be expected to die immediately, but within 3 months only 29 people died. However, we should not rejoice because this is due to many factors that are not under the control of the human being:

The explosion of the nuclear power plant caused the launch of the radioactive fog up to 10 km high, the radioactive fog that weather conditions drove away from the villages of Pripiat and Kiev, where most of the people were at home at the time of the accident and it did not rain. And finally, the radiation was not released immediately, but for 9-10 days.
It is very difficult to predict long-term effects, since the dose that each one took and all the measures that were taken are unknown.
The number of deaths from cancer can vary between 5,100 and 500,000. According to those of the U.S. Department of Energy. This figure can reach the 28,000. One important fact would be that half of these cancers would occur outside the Soviet Union, which shows that nuclear accidents can have international consequences.
Another consequence can be expected of pregnant women at the time of the accident. According to the U.S. Energy Section, 700 children are expected to be affected by the Chernobil accident (2% more than normal) and 1,900 with genetic anomalies (0.001% more than normal). Again, about half of these cases are alien to the Soviet Union.
We know that we have not talked about many points, but you can also write the entire book on this topic.
Our goal has been to show the limited role of the most advanced medical measures in nuclear accidents.
It can be said, before finishing, that the workers of the nuclear power plants can have tests of compatibility and that those who have more risk, perhaps they can keep their cryoconjelate bone marrow, since after an accident it is very difficult to have the compatible bone metrics between donors and be able to transpose their deconjelated bone marrow.