Tissue engineering: creating new bone

Orthopedic surgeons have become experts in sewing and immobilizing fractures by killing them. In recent decades they have also learned to introduce bone fragments from elsewhere to repair major damage. However, some fractures do not support vaccines or there are no bones suitable for vaccines. Therefore, in the USA and Europe is investigating new ways to replace broken bone: biomaterials vaccinations with molecular signals, bone marrow stem cells and gene therapy. These are the leading lines of research in textile engineering.
Molecular scaffolding: matrices

One of the lines of research is intended to use artificial matrices as scaffolds so that the bones form themselves. Most of the research is in the experimental phase, but there is already a product pending authorization by public administrations. It is a collagen matrix, which contains a natural protein that generates the signal that sends certain bone cells to start regenerating.
For many years, surgeons have used collagen and hydroxyapatite supports to bind the fractured parts and have the body repair the wound itself. The technique was adequate, especially in minor fractures.
Now, however, researchers work at Rice University in Houston and at the Mayo Clinic in Rochester, in Minesota, around a polymer pioneer injecting into the place to form. The precursor polymerizes immediately after entering the fracture, becoming a porous matrix that supports new bone cells. As the new bone forms, the matrix is undone and becomes a natural metabolite that will expel the bodies on its own. In animal testing, it has been proven that these polymers provide bone with mechanical strength, in addition to growth, and are fully biocompatible. In addition, the results are even better if a new matrix support is placed.
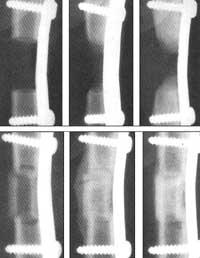
But the bone is not made by the matrix itself, but by mixed proteins, called bone morphometric proteins (BMP). In the 70s, a protein from this group was isolated for the first time, but until 1989 they did not manage to clone (specifically the protein BMP-7) and in the 90s began to use this group of proteins for bone repair. In 1992, the first attempt was made with humans on a bone fracture that was not formed for 9 months. The result was very good, equal or better than those previously obtained by introducing healthy bones from patients.
But all great hopes have their indentation, and this method also has limitations. According to some researchers, in natural processes, a few BMP nanograms per gram of bone matrix are sufficient to initiate bone repair. However, when you want to start this repair artificially, micrograms per gram of artificial matrix are needed (six times more, approximately). No health problems have been detected, but treatment would be much more expensive.
Gene therapy
Another option is to reach the fracture the gene that will cause bone formation through gene therapy.
The initial tests used adenovirus to bring the gene that would originate BMP-2 to the bone marrow. Later, the transformed cells grew into demineralized bone matrix and were introduced into intentionally broken bones. The damaged bone formed well. In a similar attempt with dogs, plasmid (circular part of DNA) was used to get the gene into the fractured bone. The plasmid was inserted into a polymer matrix and into a hole in a dog's bone. The surrounding cells assimilated the plasmid and expressed it for about six weeks. The bone formed immediately.
Tests with humans are now being prepared.
Source of new cells

However, some researchers have a headache: the shortage of stem cells in the broken place in the two previous techniques can be a problem. Although injected signal molecules reach the stem cells of the place to repair and manage to separate them, it may happen that there are not enough stem cells to heal large wounds. Therefore, several groups try to replace natural stem cells with others grown in the laboratory.
Unlike embryonic stem cells, bone marrow stem cells, also called mesenchymal stem cells (MSCs), are unable to transform into any cell. They will become bones, cartilage, and tendons or crines, as well as nerve cells in the heart, muscle, and spine. Although stem cells occur throughout animal life, it seems that the amount decreases with age. And that is not the best for those who have lost large pieces of bone.

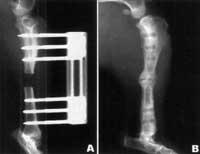
Animal studies have shown that BMP treatments have problems filling and filling bone gaps greater than 25 centimeters, as they are not enough stem cells. In these cases, BMPs begin to ‘catch’ the stem cells by the edge of the healthy bone and create the new bone toward the center of the hole, but no bone grows in the core of the matrix. The problem is the same if healthy bone is taken and injected, if there are not enough stem cells.
Therefore, stem cells have begun to enter the direct repair area of the Baltimore CEO of Osiris Therapeutics. By 1990 the stem cells of the bone marrow were deposited in a porous ceramic substrate based on calcium and managed to form fractures of 8 millimeters. Later they worked with larger animals and today they want to try with humans. So far they have achieved good results with mice, rabbits and dogs. Other research centers have similar results.
The problem with this technique is time and therefore money. At the moment, the patient must be removed stem cells, raised in the laboratory and incorporated into the same patient, which requires time. Therefore, the Osiris are experimenting with the hope that they will take one animal and enter another. In fact, bone marrow stem cells do not have markers that identify T cells in vaccine rejections. They say that they have managed to integrate the cells of mice and dogs and that, in addition to not producing rejection, the bones have grown normally.





