Assisted reproduction in women with cancer
In recent decades, there have been significant improvements in oncology treatments, which has led to increased rates of cancer healing. However, cancer continues to cause numerous damage to the reproductive system. This side effect varies depending on the age of the patient, his or her personal fertility status and treatment (drug used, dose, duration of treatment). Taking into account all these factors, the toxicity of gonads will be partial or total.
Fortunately, along with cancer research, assisted reproduction has also taken great steps and, together with the knowledge of both areas, women with cancer can have children.
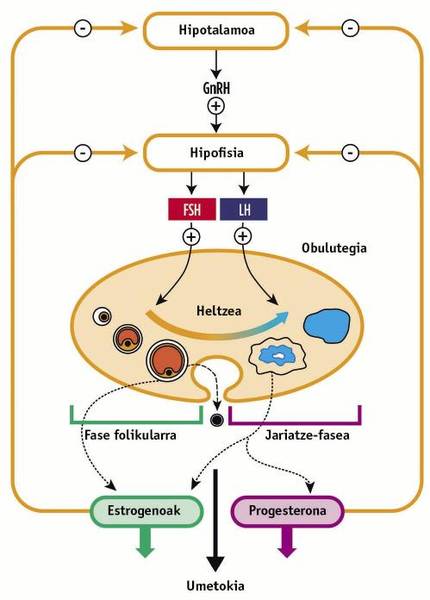
Hypothalame-hypofiso-ovary axis
Two endocrine brain glands, hypothalamus and pituitary, control the function of the ovary in two phases: the follicular phase and the secretion phase. The follicular phase covers the first fourteen days of the woman's monthly cycle, until ovulation occurs. The second phase comprises the following fourteen days until the beginning of menstruation.
At the beginning of the rule, the hypothalamus sends to the pituitary the gonadotropin secretion hormone (GnRH), causing the secretion of two hormones: the follicular stimulating hormone (FSH) and the luteinizing hormone (LH). The first is poured on the second or third day of menstruation and stimulates only one of the ovarian follicles for fourteen days. As a result of this stimulation, the obocito that arrives, through an enzyme called aromatase, produces sex hormones: estrogens (estradiol and estriola) and progestagen (progesterone). In the middle of the cycle, by increasing the level of these sex hormones, LH secretion occurs in the pituitary and maturation and ovulation of this follicle. The follicular phase ends then.
The rest of the obocyte free follicle remaining after ovulation in the runoff phase is called the corpus luteo. The corpus luteum will continue to secrete estrogens and progesterone to prepare the uterine endometrium for fertilization. On the other hand, high concentrations of sex hormones cause negative feedback in the hypothalamus and in the pituitary to avoid an excessive amount of hormones. If there is no fertilization, the decrease in FSH and LH levels will cause the expulsion of the corpus luteum and endometrium through the rule, taking the cycle to zero (see figure 1).
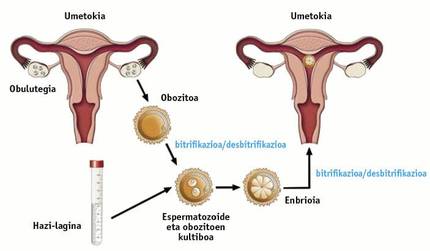
In vitro fertilisation treatment + vitrification
Although there are several techniques to protect the fertility of women with cancer, the sum of in vitro fertilisation and vitrification is considered one of the best, in view of the results obtained.
Through in vitro fertilisation, the natural reproduction of the body is artificially reproduced in a laboratory. The goal is to extract sexual cells to man and woman, create embryos and then insert them into the uterus to the patient who wants to become pregnant.
As mentioned above, in normal conditions, in the sexual cycle of the woman, a single follicle is ovula every month.For in vitro fertilisation, a process of ovarian stimulation is launched in order to reach more than one periodic follicle and have more possibilities to reach the goal. For this treatment, galenic preparations composed of: FSH and GnRH antagonists. The first causes a greater secretion of estrogens and an increase in follicles. The antagonist of the hormone produced in the hypothalamus, on the other hand, inhibits this gland and, therefore, interrupts the secretion of FSH and LH in the pituitary. Therefore, it is essential to introduce high doses of external FSH to stimulate the ovary. It is recommended to begin treatment the first three days of the rule to take full advantage of the follicular phase.
The generated obocytes are extracted by a transvaginal puncture and then incubated in a culture medium along with the sperm. In this way, the embryos that arrive at the final maturation phase are inserted into the uterus of the patient to be fertilized.
To protect the fertility of patients with cancer, both oocytes collected and embryos generated must be vitrified (frozen) before starting oncological treatment. When the patient exceeds the cancer, oocyte or embryo devitrification and placement in the woman's uterus will be performed (see Figure 2). This is the best way for women with cancer to have children.
Vitrification is very fast for ice crystals to form and do not damage cells. For this purpose liquid nitrogen (-23,000 °C/minute) and cryoprotectors are used. Once vitrified, oocytes and embryos can be maintained for hundreds of years.
Hormonal Cancers Hormonal Cancers
Among hormone-dependent cancers are endometrial and breast cancers, with breast cancers being the most common malignant tumors in women.
These cancers, unlike others, need estradiol to develop and tumor cells would die without estradiol. At a higher body level of this sex hormone, it is easier for the proliferation of cancer cells.Follicular stimulation derived from the treatment of in vitro fertilisation is, therefore, a problem in women with these diseases, since this stimulation also increases the levels of estradiol.
In the ovary there is an enzyme called aromatase, necessary to produce sex hormones by gonadotropin. This enzyme uses FSH and LH hormones to carry out its work, both naturally generated by the woman and artificially introduced by the outside.
In hormonal cancers, aromatase inhibitors are used to prevent the increase in estradiol levels. In addition, the patient should receive a cycle of habitual treatment of in vitro fertilisation. In this cycle, due to the influence of aromatase inhibitors, a smaller number of follicles are stimulated than in women with other types of cancer, but sterility by gonadotoxicity is avoided. Therefore, women with endometrial or breast cancer will be able to produce less obocytes and embryos and, consequently, vitrify them, but enough to become pregnant.
Time of treatment
A woman with cancer, before starting a cycle of in vitro fertilisation treatment, should know the type of tumor it presents and the date of oncological treatment. The date of the last month of the patient will also be taken into account. All these data are necessary to select the treatment strategy of in vitro fertilisation.
If before starting oncological treatment there is enough time to start an in vitro fertilisation cycle and stimulate the ovary, there is no problem. But sometimes, unfortunately, there is no time and the process of stimulation must be shortened. For this reason, it is common for patients to initiate ovarian stimulation outside the first three days of menstruation. In these cases, GnRH antagonists and several doses of FSH are used to take the measurement, even if the woman is in phase of menstrual cycle secretion.
If the patient needs immediate oncological treatment, the only option is to remove and vitrify the ovarian tissue using laparoscopy. This technique, however, has the risk of finding malignant cells at the time of tissue transplantation, so its use is exceptional.
Looking to the future
The protection of fertility is increasingly important due to the increase in the rates of morbidity and cure of cancer and the delay in the decision of parentage couples.
When a fertile woman learns she has cancer, she launches a series of emotion-filled reactions, like any other person who gets unhappy news. He begins to worry about his survival and is affected by a strong anguish, disappointment and sadness. As if it were not enough, if you want to have children, you must make the decision to become a mother without delaying too much time to delay the oncological treatment as little as possible and begin in vitro fertilisation as quickly as possible. However, according to some studies, the possibility of protecting fertility and looking to the future with the eyes of motherhood gives them peace and hope in those hard times. Therefore, assisted reproduction techniques must always be presented and never abandoned.
Healthy women with a family history should be presented with the technique of fecundation and in vitro vitrification as young as they wish. Since vitrified oocytes last many years, prevention would be better if we start at earlier ages. For example, if a twenty-two-year-old woman vitrified her oocytes and then, at thirty-five, suffered cancer, these obocytes will continue to be twenty-two years old. In this case we would have better quality oocytes and probably more. In addition, we would cut the treatment of in vitro fertilisation and earn time to fight cancer. Through genetic analysis, women who might be interested in it could be detected.
Avoiding long-term vitrification of oocytes will be one of the main challenges of science. This would be achieved through genetic engineering, creating an obocito from a healthy cell. It is already being investigated how to remove a heart, muscle, or eye from a fibroblast from the arm, why not an obocito? It is clear that today it is still not possible, but, seeing at what speed science advances, we can address the hope that it will become a reality in the future.