Blood selection for transfusion. Blood Groups Blood Groups
Although some of the blood transfusions that were initially performed between humans were beneficial, most of them resulted in the destruction of red blood cells or hematins. Since then, much progress has been made in this field and today everyone knows that each person has his own blood group and that, depending on this, they will choose, if necessary, the blood for transfusion. To begin the work we will publish on blood transfusion, we will mention what are the blood groups, how many there are, what is their importance and other points.
Basic concepts Basic concepts

The cells we have in our body are known in our defensive or immune system, so this does not have to act against them. However, bacteria or viruses that produce the infection contain unknown substances of the body in your membrane or skin and the immune system will produce anti-infectious substances.
These infective agents are called antigens and antibodies to substances produced by the immune system against them. If in the membrane of red blood cells or erythrocytes there are also antigens and the antigens of another person's erythrocytes are not like ours, we will produce antibodies against them. Antibodies are special proteins called immunoglobulin (Ig). Five types of immunoglobulins are known: G Ig, M Ig, A Ig, D Ig and E Ig (the last two unimportant in blood transfusions).
Blood Groups Blood Groups
In the erythrocyte membrane there are numerous different antigens and when a group of antigens is independent from the other we say it forms a system of blood groups. The most well-known systems among the population are undoubtedly the so-called ABO and Rh and, since they are the most important for blood transfusion, we will talk about them.
This was the first system of blood groups that were found and is the most important one today. The groups and subgroups that can be made according to this system, as well as the antigens and antibodies associated with them, can be seen in Table 1. Two antigens. You can say: A (can be A or Al) and B, and depending on whether or not there is:
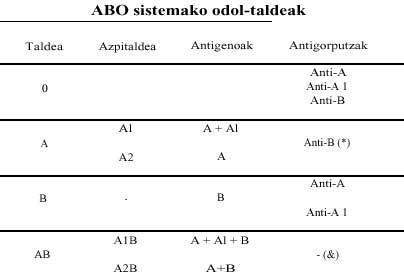
- Group O: Erythrocytes do not have antigens A or B. Therefore, this group does not know these antigens and generates contrary antibodies. 43.5% of the population of European countries belongs to group O, while the percentage of Euskal Herria reaches 53%.
- Group A: has two subgroups (Al and A2) and since these people do not know the B antigen, they have anti-B antibody. As group O has no antigens, there is no anti-O. In Europe group A presents a frequency of 39.2%, equivalent to 40% of the Basque Country.
- Group B: The B antigen can be inflamed in the erythrocyte membrane of these people, producing anti-A (anti-A and anti-A1). This group is more frequent among Europeans than among Basques, since the percentages are 12% and 5% respectively.
- Group AB: Antigens A and B appear in erythrocytes and as these people are known by both antigens, they do not produce antibodies. In this group, two subgroups can also be distinguished as shown in the table, i.e., subgroups A1B and A2B. This group also appears to a lesser extent among the Basques: 1.4% compared to Europeans. It is expressed in 4.5%.
Almost 80% of people of white race produce substances similar to the antigens of the blood group through certain glands (such as those that produce saliva), whose study allows to know the blood group to which they belong.

Newborns have no antibodies and begin to form anti-A and anti-B at 2 or 3 months. They are called "natural" antibodies because they occur without the influence of any antigen. They are mainly of type M Ig and to some extent of type G Ig and A Ig. If an incompatible transfusion is performed, more G Ig would appear.
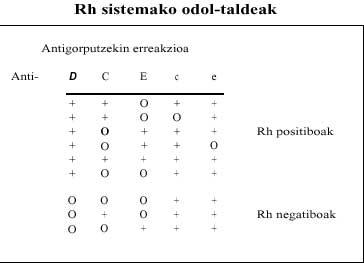
This system is more complicated than the ABO system, although it is limited to saying that it is positive or negative at normal level. To make it understandable, I will say that in this system there are combinations of various antigens. When we are born, we receive information from each of the parents of three antigens, which makes us have six antigens.
These antigens appear by couples, so we can distinguish three pairs: D and d, C and c, E and e. Antibodies against anti-D, anti-C, anti-c, etc are also known. But there is an exception, since anti-d has not been found and therefore with d means that there are no D antigens. Table 2 shows the most common combinations.
Antibodies against the Rh system do not appear spontaneously in children, that is, just as those of the ABO system are not natural; those of the Rh system appear after an incompatible blood transfusion or pregnancy (as we will see in another work).
The D antigen is the strongest antigen for the formation of antibodies and therefore, while not specified otherwise, it means that a blood is positive Rh and has D antigen, while the negative blood R h will not have D antigens. Then, antigens with higher immune response strength or antibodies are E and c. Although the antibodies of this system are initially of type M Ig, then appear mainly of type G Ig. The positive Rh represent 85% of the European population and the negative 15%. In the Basque Country, 24.4% are negative Rh and 75.6% positive Rh.
Other systems
As I mentioned above, many different systems are known, but their importance is less than that of those mentioned above. However, they are very important to find adequate blood for some people, and that is why hematologists take them into account. Since we do not want to delve into this work, we will limit ourselves to making a mere mention of some systems:
- Lewis System: It is formed by Lea and Leb antigens. The 72% of white people are Leb.
- Kell system: The most important antigens are K and K, with 91% of the total blood.
- Kidd system: It is formed by JK and JKb antigens.
- Duffy system: in this group are two the most important antigens: Fya and Fyb.
- System P
- MNS system
- System I-i: In the blood of the umbilical cord of the newborn is the antigen i, but at 3-4 months begins to appear the antigen I and most adults are positi bos, while the antigen i is lost and the adults are i negative.
Blood selection for transfusion
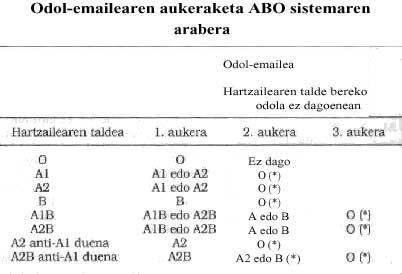
When we are going to transfuse a person, the first step is to know what his blood group is. This means that we need to know which group the ABO system belongs to and whether Rh is positive or negative. Once this is known, we will choose in the blood of the donors that belongs to the same group, according to what we can see in Table 3.
For those of group O we will always have to choose the blood of group O and on the contrary, the blood of group O can serve for those of group A, B and AB. Therefore, group 0 is considered the most universal donor. However, those in group O have anti-A and anti-B antibodies in the blood plasma, so it is advisable to remove the plasma before transfusing the blood to remove the antibodies.
For those of group AB the blood of group AB will be chosen preferably, but when it is not in the blood bank it is possible to give the blood of group A or B and in its defect the blood of group O. For these reasons, the AB group has been called universal receptors.
On the other hand, we will give the same blood to the positive Rh and in their absence it is possible to give negative Rh. Finally, negative Rh can only take blood from the same group.
The other blood systems are not taken into account in ordinary transfusion tests if a person does not have special antibodies against them, which is unlikely.
Once the blood of the most appropriate blood group has been chosen, a final study is needed before transfusion: in the laboratory, the blood of the patient is placed together with the blood of the donor and compatibility is analyzed. This study is called a cross-test and if there is no reaction between both blood, it is said that cross-tests are negative, so that blood can be introduced. If the reaction appears, these blood is incompatible and cannot be transfused.
In the blood banks, cross tests prior to transfusion are mandatory and only in case of extreme bleeding can blood transfusion be necessary before these tests. In these cases we will use the blood of group O negative until we can transfuse the blood passed through the cross tests.





