The laryngectoof Euskal Herria can also speak
As discussed in previous articles, primary and secondary fistuloplasties have been the central focus of our study. To communicate our surgical techniques, we will focus on the same distribution.
Primary phonological fistuloplasty Á
In July 1981 we began to perform primary phonatory fistuloplasties.
While for some it is customary and successful to put a prosthesis on the fistula, for us the goal is for the patient to circulate without prosthesis.
If any surgical technique is to be maintained and extended, it must be easy to perform, fast and effective.
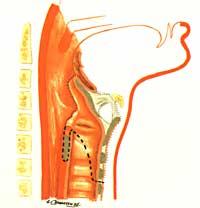
The steps to follow in our surgical technique are:
- U-cut Just like in conventional laryngectomies, the skin and muscle nerve are raised.
- Tracheotomy The type of tracheotomy for fistuloplasty is important. U-tracheotomy is done by horizontal cutting and at the bottom of the first or second tracheal ring.
- According to the state of the Ganglia, we will proceed to its emptying.
- Larynx removal First the larynx, including the hioid, is removed from top to bottom and then, if necessary, from bottom to top.
- If during removal of the larynx the cricoid seal has been preserved, we will cut through the scalpel all the upper corner of the mucoperichondria and release it down to the lower edge of the cricoid. At that time the cricoid is extracted.
- Doing the fistula is doing the fistula (if we want it to work and close well) as best as possible, it is the most important step of our technique.
- Musculoplasty The cryopharyngeal muscles contract back when they are cut off from their cricoidal implant, that is, to the sides of the esophagus. Therefore, we must seek them and paint them. Then we take the ends and take them in the center line. In this way they are very daring about fistula.
- Fistuloplasty coating The muscles sewn in the center line will be covered.
- Placement of the probes (K-31) in the fistula we introduce a fine feeding tube for children.
- The Tunelizaci??n at the top of the MucopericondrÃa gives two or three points per finger and we build a term. This tunnel should be able to form a large tracheostoma and that the fistula is not very hidden in the upper part of the tracheostoma.
- We close the pharynx so that there are no pharyngostomas at the level of the pharyngo-esophageal mucosa we do two seams. In our experience no pharyngostomas occur.
- Flat stitchingDecreased skin and muscle nerve. In the place where the nodes were placed the redoyas and we started by the line of half seam and with fine silk, at first. The skin is sewn to the mucoperichondria and the upper part of the tracheostoma is formed. This surgical technique has improved swallowing and few prostheses had to be placed. Only 14% of patients needed prostheses. The patient treated by this technique may talk by covering the tracheostomy with the finger or by placing a fonatorium valve. If necessary, a silicone tube will be placed in the traceostoma. This improves the coverage of tracheostomy and therefore the quality of the voice.
Secondary phonological fistuloplasties
In this section there are two types of cut:
- Secondary fistuloplasty of tracheal climbs
- Secondary Tracheal Puncture Fistuloplasty
Let's analyze these two types of cuts.
Secondary fistuloplasty of tracheal climbs
This technique began to be applied to patients who at the time of total laryngectomy did not remove the cryoid, since these patients could not be applied the tracheal puncture technique. Seeing the good results of this technique and seeing that the patient could circulate without prosthesis, we began to apply cricoid to the patients removed.
The surgical technique is similar to that we have exposed in primary phonological fistuloplasty.
If the cricoid has not been removed previously, it is released until the first tracheal ring. If there is no cryoid it is released until the second and third tracheal ring.
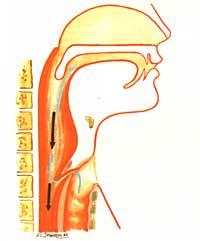
In the back wall of the trachea we make a vertical cut of 8 mm in length, leaving the top between two and three millimeters. Here, with the same technique used in primary phonological fistuloplasty, fistula is formed with the esophagus.
The replacement of tracheal puncture by this technique is because the patient can circulate without prosthesis. However, when tracheostomas are very small, the patient may perform a tracheoesophageal puncture when the tracheoesophageal wall is very wide or the pharyngoesophageal pathway is narrow.
If patients already have some erygmophonic voice, they should understand that after the cut they should not swallow air (but use air from the lungs). Patients quickly acquire this new fonation mechanism. However, they keep the voice erygmophonic and can use it whenever they want. Some patients claim that their voice has improved after cutting.
As it is an operationally worked fistula, it will usually never close. Although they need a prosthesis to eat or drink, they can be removed to sleep or speak without risk of fistula closure.
In the case of patients who are going to put prosthesis, it is very easy to put it, since the fistula is always open and the prosthesis is short.
Without prosthesis, it absorbs well two thirds of patients and only one third needs swallowing prosthesis.
Secondary fonatorium fistuloplasty of tracheal puncture

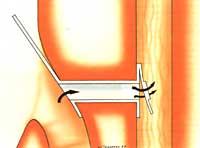
In 1981, following the SINGER-BLOM method, we began to apply the tracheal puncture technique. If the patient is placed in supine decubitus and begins with general anesthesia, local anesthesia is currently used.
In this way, this surgical technique can be applied in a traveling way and consists in the fact that the patient knows after the intervention, remove and put the prosthesis and cover the tracheostomy well with the finger.
The technique is very simple and is done in five minutes.
At the place chosen for the puncture is injected 1 cm 3 local anesthesia.
A teflon tube is inserted through the mouth and from this tube the fibroscope to see the needle for puncture.
The needle catheter is inserted through the tube until it is seen through the mouth.
Then we open the fistula and place the prosthesis there. This way the patient can start speaking immediately. This technique can be used under general anesthesia when the circumstances of patients require it.
This technique is simple to perform and the surgeon does not require any special skill.
The voice that is achieved is better than the best voice erygmophonic.
The success rate ranges from 80% to 90% and can be higher if expectations are met properly.
Phonetic prosthesis
The first phonatory prostheses were presented by SINGER and BLOM in 1979 in the USA. Since then several prostheses have appeared on the market and at this time there is a German, a French, a Dutch, an Italian, some Americans and ours, which we published in 1983.
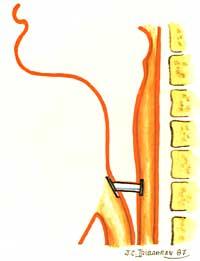
Our prosthesis is silicone and we have made models of two diameters and three lengths. This prosthesis has no itching, neither in the trachea nor in the esophagus and its protective mechanism is membranous.
While some prostheses will be modified by the doctor, the patient may change ours. In this way the patient becomes independent of the doctor.
The prosthesis is used in secondary tracheal puncture techniques and in tracheal lift techniques with fluid leakage.
Fonatory valves
The problem of all surgical techniques is the formation of tracheostoma. Therefore, in order to anchor (pronounce) it will be necessary to cover the tracheostoma.
The easiest way to close the tracheostoma is by using the finger, but this practice generates certain discomfort. On the one hand, the use of a fonation hand means that you cannot use that work hand. On the other hand, if the hands are not clean it is not hygienic to cover the tracheostomy with the fingers.
Therefore, new tracheoostoma coating systems have appeared. At this time there are four different models on the market: the two Americans, one German and the other English. The fonatory valves prevent the patient from periodically placing the finger on the tracheostomy.
Phonological results of phonological fistuloplasties
One of the most important consequences of these cuts is the lack of rehabilitation to speak, as patients learn to speak immediately.

As for voice quality, this factor is measured in several parameters.
- Intelligibility The voice of patients who have undergone phonological fistuloplasty is very understandable when speaking on the phone, despite the noise. The pronunciation of phonemes is clearer than with the erygmophonic voice.
- The frequency varies from patient to patient. Even a patient can change the frequency to their liking. Some can also sing.
- Hobby and rhythm As you don't have to swallow air and you can use the air in your lungs, the rhythm is similar to the natural voice.
- Intensity The intensity of the fistuloplastic voice is greater than that of the erygmophonic voice. While the intensity of the first varies between 70 and 95 dB, the second varies between 57 and 70 dB.
- Acceptability The fistuloplastic voice is much more acceptable in society than the erygmophonic voice. The patient also feels more satisfied with the fistuloplastic voice than with the erygmophonic voice. From a clinical point of view, the results are variable and depend on the criteria of the operating rooms.
We have manufactured 300 fistuloplasties, of which 175 primary and 125 secondary fistuloplasties. The success rate was 85%. These results are quite good to follow this path.
This series of articles on laryngectomy ends here. A disease that in its day caused death. Today, life has passed.
Translators: J. Aizpurua Sarasola and J. Agirre






