Resistance to antibiotics from the perspective of Single Health

Nafarroako Unibertsitateko irakaslea eta mikrobiologiako katedraduna eta Salud Global (Osasun Bakarra) liburuaren egileetako bat
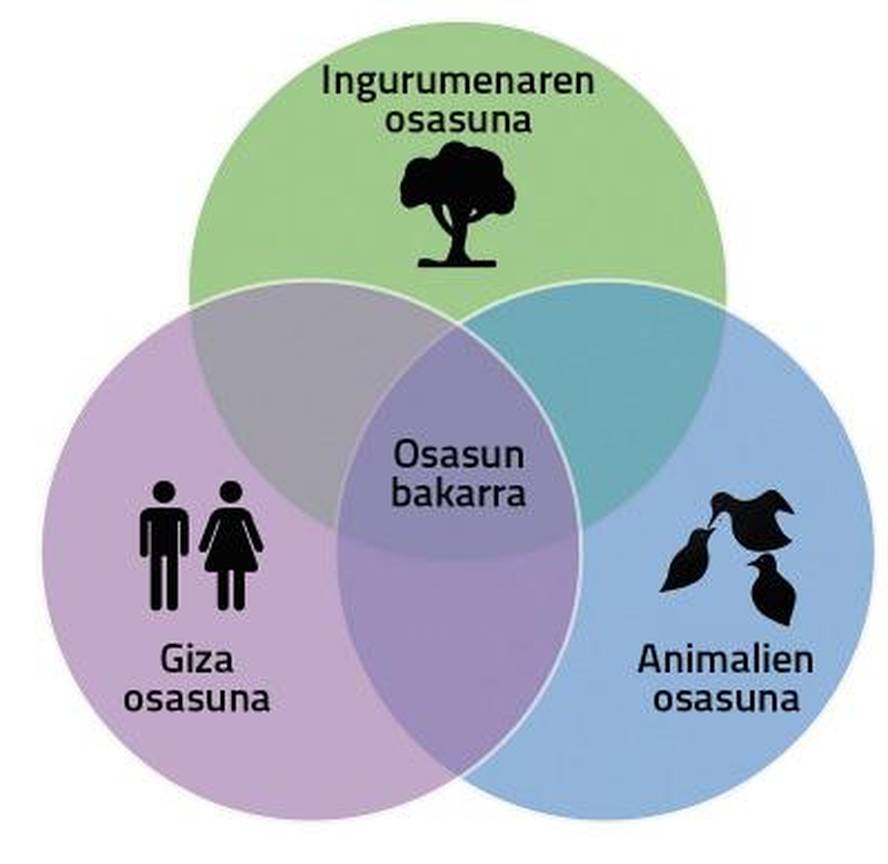
Antibiotic resistance is a global problem affecting human and animal health and has to do with the presence of antibiotics in the environment. This interrelationship is Single Health or Global Health.
In veterinary medicine, antibiotics are essential for the treatment of infectious diseases, both in production animals (livestock, poultry, pigs…) and in domestic animals. In some cases, antibiotics are used as preventive measures, particularly in intensive animal husbandry, to help prevent infectious outbreaks and reduce the spread of pathogens. Although banned in Europe, low doses of antibiotics for long periods of time are often given to animals in some countries to enhance their growth and improve their food efficiency. Therefore, the indiscriminate and abusive use of antibiotics in veterinary medicine implies the development of resistance. Therefore, responsible use of antibiotics in veterinary medicine is essential: the appropriate medicine must be chosen, the appropriate dose determined and the duration of treatment. In addition, as identical or similar antibiotics are used in human and veterinary medicine, resistance to antibiotics developed in animals can pass to humans and vice versa. It is therefore vitally important to use a comprehensive approach to address the problem as a whole.
On the other hand, it is rarely taken into account that the “life” of a drug does not end when it is expelled from the patient’s body. The remnants of antibiotics from animal production, excretions and human and animal waste accumulate in and contaminate soil and water. For example, effluents from wastewater treatment plants present significant concentrations of antibiotics, and residues of manure antibiotics contaminate soils and end up in aquifers used for irrigation and fertilization of crops. The presence of antibiotics in natural environments creates an environment conducive to the development and reproduction of resistant bacteria. Bacteria are able to transfer their resistant genes to other bacteria. So as resistant bacteria multiply and expand in the middle, resistance increases.
The genetic dispersion between bacteria of animal and human origin is of public health concern. To work on this aspect, it is necessary to develop more stringent regulations and actions in waste management and to develop a comprehensive vision that analyzes problems from their origin. In this strategy, monitoring and monitoring of resistance to human, animal and environmental antibiotics is a key issue. Interdisciplinary collaborative research is essential for the development of new drugs and technologies that take into account antibiotic resistance. The search for and promotion of alternative therapies can also be effective in humans and animals. Development of joint training policies and programmes in human and veterinary medicine. Essentially, solving the problem of antibiotic resistance requires the collaboration and coordination of human health, veterinary and environmental professionals. The Single Health Strategy is the best way to combat the threat of antibiotic resistance.