The same mutations that protect against infections increase the risk of other diseases
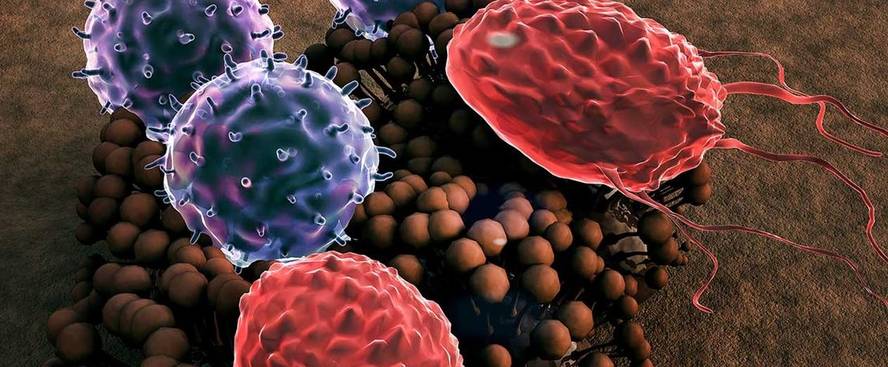
Dutch researchers have studied the consequences of coevolution between pathogens and the human immune system and found that genetic variations that help fight certain infectious diseases aggravate the risk of certain inflammatory and autoimmune diseases. In addition, they stressed that currently the immune system continues to evolve depending on the place of residence and lifestyle of people.
Researchers recall that inflammation is one of the most effective responses to fight infectious diseases. And as in the past life expectancy was shorter, the inflammatory and autoimmune diseases that occur throughout life were not so influential. Therefore, mutations that protect against infectious diseases have been prioritized throughout evolutionary history. They also highlighted the origins of human groups and the influence of migrations.
For example, the malaria parasite has infected African populations for thousands of years. Therefore, evolutionary processes have selected the DNA of people resistant to infections. This is because, along with endurance, they are more likely to develop cardiovascular disease. Thus, current Africans tend to develop arteriosclerosis and other cardiovascular diseases.
For their part, some Neanderthal hereditary populations have a mutation that gives them some resistance to HIV, which increases their risk of asthma, allergies and other autoimmune diseases.
Current examples include the difference between an African hunter-gatherer group and an urbanized African-American group: as they acquire Western lifestyle habits they tend to develop type 2 diabetes.
In addition to demonstrating that the methodology used is suitable for this type of conclusions, researchers have recognized that there is still much work to be done, since only limited human groups have analyzed it. The results have been published in the journal Trends in Immunology.