Arthroscopy
As a definition, arthroscopy is a technique for visualizing the body or intraarticular joint using an optical instrument.
Arthroscopy is generally used for two main purposes: diagnosis and healing, one for diagnostic arthroscopy and one for therapeutic or surgical arthroscopy.
In diagnostic arthroscopy, the goal is to obtain an accurate diagnosis through the optical tool, by clearly observing the inside of the joint. Therapeutic arthroscopy is the next step. Once the pathology is determined, with the same technique it recovers, apart from the classical intervention.
In most cases diagnosis and therapeutics are performed successively, that is, immediately after diagnosis the treatment of arthroscopy is proceeded.
History of Arthroscopy
XIX. In the 20th century, the first investigations and analysis of body cavities were initiated through optical escopy. Bladder, vagina, rectum, pharynx, etc. were inspected. However, the first sessions of optical escopy to see the joints did not begin until 1918. It was then that the Japanese Kengi Takagi began to perform the first arthroscopies at the University of Tokyo with his first arthroscope without lenses. Takorri's intention was to make an early diagnosis of joint tuberculosis.

After the lockers, different models and applications of arthroscopes were developed around the world. In 1925 Krensche carried out and presented for the first time the arthroscopic investigation of meniscus. Between 1931-35, Burman dedicated important works in this field. Also Sommer in 1937, Vaubel in 1938 and Mayer and Wicker in 1939.
However, in the advance of arthroscopy, two aspects must be taken into account: on the one hand, the technical improvements of the same apparatus (technical, optical and engineering) and on the other, the one related to the results of medical research. As we have already mentioned in the previous lines some names of medical research, we will take a look at the advances in the technical part of arthroscopy.
The first arthroscope, that of Takorri, was without lenses and with it you could see very little.
Watanabe's 21st arthroscope had lenses and offered the ability to see face to face. The arthroscopic study of the joint was carried out inside a stream formed by serums or distilled water to keep the joint interior clean. The optical apparatus, on the other hand, had to cool down to prevent the burning of the articular tissues. This arthroscope was presented in 1960 and two years later Watanabe himself performed the first surgical arthroscopy. A broken meniscus is cleaned by arthroscopy without usual knee intervention.
The last step was the arthroscope of O´Connor. This tool, presented in 1970, in addition to facilitating diagnosis, extends surgical possibilities. The current arthroscopes are just a continuation of the O´Connor arthroscope, or what is the same, we are in the O´Connor generation.
The success of arthroscopy is based on two main points. On the one hand, the materials have been greatly improved (the optics have been improved, the cold light is used, the video is used and the devices have been miniaturized) and, on the other, the procedure and the ability of the arthroscopy has been completely modified. Previously it was only seen, but now with the exploratory key the structures are touched. The instrumentation for the manipulation of tissues and anatomical structures has improved and sophisticated notably and can currently be operated as the knee: meniscus, cartilage, synovial, ligaments, etc.
Currently arthroscopy is becoming a basic technique in orthopedic services and has applications in rheumatology, sports medicine, research, etc.
Description and fundamentals of materials
The devices used in arthroscopy are the arthrosscope, the fiberglass cable, the light source (which generates cold light), the video system, the surgical tool (can be motorized or not) and other devices. We will now analyze individually:
1. Arthroscope
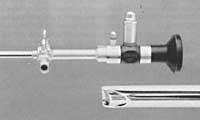
The optical system of the arthroscope has two functions: capturing the image and bringing light to the joint cavity.
The forms of image collection vary according to different types of arthroscopes, but usually the entire arthroscopy tube is a thin, long lens.
In fiber optic arthroscopes, this thin, long lens is surrounded by fiberglass to drive and move light into the cavity. These two elements are inside a metal cap.

There are arthroscopes of different caliber or size, some of them used in larger or larger joints (for example in the knee) and others in small joints (ankle, elbow, wrist). The main joints are 4-6 mm and the small ones are 2 mm.
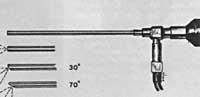
The final end of the arthroscope optical system can be of different angles:
- with an inclination of 0º, that is, with the straight direction of the image area.
- With an inclination of 30º. The direction of your image area is tilted 30º and the turn allows you to see an area up to 70º.
The arthroscope rests on the shirt. It is a protective tube with the following functions:
- Offer metal protection due to fragility of the optical system.
- Conduction of serum or cleaning distilled water from the concentric space between the optical system and the portal to the joint. The inlet and water regulation shirt has at its end some valves.
2. Fiberglass Cable
This system transports cold light from the source where it is generated to the arthroscope. The gauge of the cable depends on the power of the light source.
3. Light source
The cold light generating source can provide different powers depending on the work to be done. The power required for diagnosis is 150 watts and the power required for video-arthroscopy (currently most used) is 250 watts.
4th Video System
It consists of two components: camera and monitor. There are cameras of different models, but they have the following common characteristics: they are small (easily usable with one hand), are light (almost all of less than 200 grams), can be sterilized by liquid immersion and can regulate the temperature of the light (currently the regulation is automatic).
5. Surgical apparatus
The surgical tool can be non-motorized or motorized. We will first describe the non-motorized components and then the motorized components.
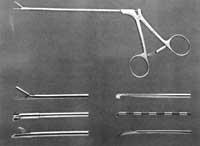
Non-motorized components are:
- Exploratory key. It is the most basic tool for exploratory study or diagnosis when starting arthroscopy. Represents the surgeon's hand.
- Tweezers basket. There are several gauges and angles depending on the needs. The clamp is cleaner. When it is necessary to remove damaged or cracked anatomical structures, the following clamps will be used. As if it were a bite, damaged structures are curled into very small pieces by a tube.
- Scissors. They work before the basket tweezers. The scissors are also of different caliber, design and angles.
- Kneading or pressure clamps. They are used to remove relatively large parts within the joint that cannot be removed by absorption. They are also used for the extraction of cartilage free parts and foreign bodies.
- Scalpel for arthroscopy. Its use is reduced due to the difficulty of internal control of the joint and, sometimes, the need for new windows.
In the motorized surgical device, the work is done by taking advantage of the force of the motor rather than by cutting. The motorized surgical tool may contain:
- Sinobiotome. It is used to clean the synovial and cartilage sick or in poor condition.
- Cutting. It is the result of the evolution of the syobiotome. It is used to cut and extract pathological structures.
- Strawberry. Cleaning by infringement procedure.
6º Other tools
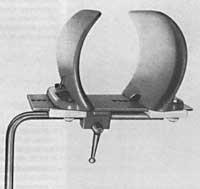
The arthroscope also has two auxiliary tools. On the one hand, a tubular system in the form of “Y” that hangs from the ceiling of the operating room (with two bags of three liters of serum that supply) and on the other, a tool to keep the thigh firm for knee arthroscopy.
Advantages of arthroscopy
The advantages of arthroscopy versus arthrotomy or conventional surgery are much higher and higher than the disadvantages. The important thing may be that after the operation there are fewer deaths. Arthroscopy makes the joint paralyzed in a very short time and the patient quickly normalizes his life and the possibility of complications disappears. Two weeks after arthroscopy many patients return to work.

In arthroscopy, the cut is very small, usually one centimeter. Therefore, the aesthetic problems it generates are also very small. Compared to usual operations, inflammation is less and pain. All this causes the rehabilitation to start before, when the patient gets ready to work.
Arthroscopy allows a more accurate diagnosis than before. A more objective diagnosis is made on radiology, scanner, nuclear magnetic resonance imaging, arthrography, etc. by direct detection of arthroscope disease. Side effects have also been greatly reduced; neuromas, painful and unethical scars, imbalance of the extender device, etc. for example.
Another advantage is the lower cost of hospitalization. In routine operations, the patient remained in the hospital for an average week and only 24 hours of arthroscopy.
Postoperative complications described below are much less common in arthroscopy. In addition, in some cases or pathologies, such as partial meniscectomies, it is possible to carry out very difficult techniques to apply in conventional procedures.
Contraindications of arthroscopy

Although the disadvantages and contraindications of arthroscopy are very scarce and limited, there is one or the other. In joints with problems no arthroscopy should be performed until all other painless methods are used. Arthroscopy should be the final clinical evaluation to determine the diagnosis. Before reaching the arthroscopic diagnosis it is necessary to use other non-invasive procedures, deep and precise anamenesia.
Arthroscopy should be avoided due to poor skin condition or infection outside the joint at that time.
Neither should this technique be used when arthroscopy is normally not possible by total or partial ankylosis in the joint. Nor when there is a suspended ligament.
Complications of arthroscopy
As mentioned above, one of the main advantages of arthroscopy versus usual operations is the reduction of subsequent complications. However, it may contain:
- Tool breakage. Sometimes arthroscopic devices break into the joint. They are narrow, long and risk-breaking tools in case of clumsy motion. In a survey of 9,000 arthroscopies, Mulholl's orthopaedic obtained the following data: In the cases of 0.03% the instruments were broken inside the joint and in 0.01% a conventional arthrotomy was performed to remove the internal part of the piece.
- Tourniquet paresis or nerve injury. These injuries are not just arthroscopy, but any intervention that requires the use of the tourniquet. To create paresis, two factors must be taken into account: the ischemia time (which in no case should exceed 1.5-2 hours in the lower extremities) and the patient's sensitivity to the anoxia of the nerves (parameter that we still do not know how to control).
- Infection. It may be present in any surgical technique. There are different statistics, but most indicate a level of 0.04%, that is, 100 times less than in the usual operations.
- Hemarthrosis. In common language they are called spill or spill. They are much less common than conventional surgery. The percentage of hemarthrosis is 2%.
- Thrombosis. It is usually smaller than in regular operations. According to some statistics, 0.1% occurs in cases.
- Hypersensitivity of the scar. Surgical intervention for the introduction of the apparatus produces bruises, so in some cases the posterior scar is painful. This complication is not given importance, as in a few weeks or months they disappear on their own.
- Synovial fistulas. They are caused by an infection or spill, but they are very rare.
- Condition to internal anatomical structures. Because arthroscopic devices are metallic, small tears in the cartilage are normal. These small scratches are usually cured by themselves, but in some cases, by the abrupt use of the tools or by the difficulty of the arthroscopy itself, they can be deeper.
Arthroscopy Joint
This section shows the joints in which arthroscopy is performed and its evolution. The list is as follows:
- Knee arthroscopy. It is the most in-depth and with the most prolific results.
- Arthroscopy of the shoulder joint. It is done much less than the knee.
- Elbow arthroscopy. It is still underdeveloped.
- Ankle arthroscopy. It is not yet very developed.
- Wrist arthroscopy. Only trials are carried out.
- Hip arthroscopy. Not yet developed. Rarely, only as a trial.
- Temporomandibular joint arthroscopy. It is still experimental.
Knee arthroscopy
The arthroscopy of this joint has always been a pioneer in history and evolution. There have been two reasons for this: having a large joint and being easily accessible due to its proximity to the skin.
Because the description of the entire technique of knee arthroscopy would take a long time, we will not devote ourselves too much to it. (This section would only interest experts and those who are studying the orthopedic specialty.) We will indicate a single technical aspect as it focuses on training for arthroscopy.
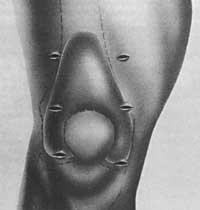
The technique of triangulation consists of two entrances to the skin that after introducing different arthroscopic devices join at the end of the arthroscope forming a triangle. The most classic example is the introduction of an arthroscope by one hole or door and one surgical device by another. Inside the joint are joined, one (optic) illuminating and showing structures when the other works. These two tools form an angle and their maintenance is usually a matter of training.

The first premise of triangulation is to see it clean. For this, the joint must be open and quiet, keeping the liquid clean. Cuts to the knee depend on the pathology to repair. Each arthroscopy consists of two (or three) inputs.
When an arthroscopic knee diagnosis is made, the entire joint must be explored in the same order. First look at the bag on the patel and the patel femoral joint. Then in the internal joint to the femoro-tibial or compartment and then to the bite between condio. Finally, the outer compartment and the rear interior are monitored.
Different surgical techniques are used in knee arthroscopy, the simplest being the following:
- Resection or cleansing of the synovial wrinkle.
- Extraction of free suprarrotulian bodies.
- Cleaning with synovium of chondromalacia patella.
- Extraction of cracked and cracked meniscus fragment.
- Extraction of the meniscus from all abrasion similar to the boiler rot.
- Release from the side altarpiece.
- Extraction of central and rear free bodies.
- Drilling and cleaning of a cartilage failure.
- Removal of tear from the posterior branch of the menis.
- Synoviectomy.
- Extraction of horizontal tearing of the meniscus.
- Complete meniscectomy.
- Treatment of dissecting osteochondritis.
- Meniscus repair and reconstruction.
- Replacement or plasty of the broken anterior cruciate ligament (autologous or artificial).
Ankle arthroscopy

Although knee arthroscopy has evolved a lot, ankle arthroscopy remains at first because this joint is smaller and narrower than that of the knee and shoulder. Therefore, to see the inside of the ankle in a simple and clear way through arthroscopy, surgeons pull the bones by traction with a nail through the heel bone, tied to an orthopedic step.
Ankle arthroscopy is recommended in cases of dissecting osteochondritis, free bodies inside the joint, chondromalacia, alterations or rheumatological defects and pyarthrosis.
Shoulder arthroscopy
Although it began to experiment 50 years ago, it had no importance until the 1970s, when knee arthroscopy developed completely. In the case of the shoulder, the development has been driven by the advance of the arthroscope and its instrumentation.
Shoulder arthroscopy does not have a complete indication. Therefore, it should be used as a last option when other forms of diagnosis have failed (anamnesis, radiology, arthrography, OTA, MRI, etc.) and therapeutic (physiotherapy, medication, infiltrations, etc. ).
Finally, the last requirement for the realization of arthroscopy (and not in any way) is that the orthopede is very skilled surgically, since in shoulder arthroscopy there are very few operating theatres, since on the one hand it is a late technique and on the other, with good results in routine operations, the habits of operating theatres are difficult to change.

Indications for shoulder arthroscopy are:
- Rheumatic disease synovitis.
- Removal of loose bodies, especially when loose bodies of bone or cartilage are in the lower area of the acromies.
- Locations. It is difficult to know the injured anatomical structure to repeat why many of the shoulder locations or chronic location. Arthroscopy can diagnose the anatomical cause of repeated mooring, so within a few days you can choose the type of intervention that can be performed to cure the anatomical lesion. Although this is a diagnostic arthroscopy, therapeutic or surgical arthroscopy has begun to spread in recent years.
- Removal of abrasions from the glenoid lip. It can be cured with therapeutic arthroscopy when chronic shoulder pain occurs.
- Shoulder Concealed. A chronic inflammatory disease can cause the shoulder to lose its ability to move and in these cases it is being experimented with the use of arthroscopy.





