The evolution of biomaterials can make reality what seemed incredible

Farmazian doktorea. Biofarmazia, Farmakozinetika eta Farmazia-teknologiako irakasle kolaboratzailea
Farmazia Fakultatea UPV-EHU, Vitoria-Gasteiz

Farmazian doktorea. Biofarmazia, Farmakozinetika eta Farmazia-teknologiako irakasle kolaboratzailea
Farmazia Fakultatea UPV-EHU, Vitoria-Gasteiz
The incidence of neurodegenerative diseases in developed societies has increased in recent decades. And although many drugs that can protect or recover neurons are being tested, there are a number of obstacles to their development and clinical administration. Among the obstacles are: (1) overcome the blood-brain barrier and reach the brain another necessary drug; (2) protect the drug from rapid degradation of the enzymes present in the blood; (3) reach the drug to the cells specifically affected; (4) increase the duration and biocompatibility of the cells available for therapy; and (5) fully demonstrate the safety and efficacy of the system to inject or inject into the central nervous system.
With the aim of overcoming these problems, scientists are making great efforts to develop biomaterials. Specifically, we are working on the design of nano and microsystems transporters manufactured with polymeric biomaterials that release neurotrophic factors (NGF, GDNF,...) to the injured zone. Five are the most important systems investigated:
1. Liposomes: vesicles formed by double lipid layer.
2. Nanospheres and nanocaps: They are spherical vesicles made with conventional solid biodegradable polymers.
3. Dendrimers: they are three-dimensionally perfect polymer networks formed by interconnected molecules around the central core.
4th Micelles: They are spherical groups formed by amphibious molecules such as cholesterol.
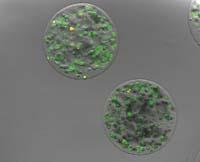
5. Three-dimensional polymeric microcapsules carrying cells: They are capsules formed by a semi-permeable layer that allows the introduction of nutrients and oxygen and the elimination of cellular waste. Due to its ease of gelification and its porous nature, alginate is the most used polymer in the formation of these microcapsules.
These conveyor systems are optimized for the release of the drug to be more effective and biodegradation is less thanks to the specific molecular coatings of the surface. This is the main advantage. In addition, the results of preclinical research carried out with these systems have been very encouraging.
Among the mentioned systems, the microcapsules that transport cells present some advantages. In fact, we assure the synthesis of neurotrophic factors of novo during the life of the cells, that is, when the factor is necessary it is synthesized at the time and also inside the patient. An example of this is the clinical trial started in 2006 in the US to treat neurodegenerative disease of retinitis pigmentosa. In this essay they have found that degenerated ciliary neurons of the retina can be recovered due to the release of scientific neurotrophic factors by the primary epithelial cells of the encapsulated retina. Noteworthy is the essay III. It passed to phase in 2009 and could soon be marketed as a drug.
However, it is still necessary to introduce significant improvements in the microcapsules that transport cells. It must be taken into account that the development of these systems is much more complex than the development of others. On the one hand, the need to design capsules that allow an adequate exchange of nutrients, residues and gases to keep cells alive. On the other hand, because to ensure safety, it is necessary to optimize the manufacturing processes.
Another of the strategies of interest that is being used in neurodegenerative diseases is the implantation of biomaterials that simulate the behavior of healthy tissue in the place of the injury itself, despite the high risk of involvement in healthy areas of the brain. In this strategy, in addition to using primary cells, interesting results have been obtained with stem cells. A clear example of this is the preclinical trial conducted by Park and members with mice in 2002. In this trial, the part of the brain was tried to recover by interruption of the oxygen flow (ischemia). For this purpose, the encapsulation of neuronal stem cells and the direct implantation of biomaterial in the affected area was carried out. They found that around the biomaterial a new nervous tissue formed by stem cells was produced, and not only that: the new neurons established connections (neurites) with other healthy neurons of the host.
A group of researchers at Emory University in Atlanta also achieved good results in 2009. Mice with brain injury were transplanted with neuronal stem cells in a biomaterial manufactured with laminin proteins and fibronectin that mimic the biological environment, and they saw that they were able to develop it, improving the loss of some brain functions.
Although the results obtained with animals are totally positive, it cannot be forgotten that working with animals and people is totally different. When we experiment with animals we use more than one animal to show that the results are repetitive and credible. Similarly, when we design the experiment, a calculation of the animals that are going to die is made to obtain the authorization of the ethics committee. But in the human being is the only choice and we can't make a mistake. That is to say, in the thousands of preclinical trials that were first performed previously, we must define all the details well, and then perform a single test in the human being to get the experiment well.
And for this we must meet many requirements. In fact, the perfect biomaterial for the treatment of brain diseases should be adaptable, biocompatible, biodegradable, chemically and mechanically stable, non-toxic, processable, capable of controlling the kinetic release of the drug and interactive with host cells. It seems that the imitation capacity of the matrix that surrounds the cells of the body is one of the keys for biomaterials to be efficient, so chemical and physical adaptations are being tested on the surfaces of the conveyor systems, looking for an interactive intelligent system with host cells.
Finally, we consider that within a few decades it would not be a disadvantage to have in hand an effective biomaterial drug for some neurodegenerative disease and to realize what three decades ago seemed incredible.





