Epilepsy and Alzheimer's Disease
Alzheimer's disease is the most common progressive dementia associated with age. Between 5-10% of people over 65 years of age may have disease, and increasing age increases the risk exponentially. Precisely, age is, along with family history, the main risk factor for Alzheimer's dementia. It is therefore clear that the aging of Western society represents an increase in the prevalence of Alzheimer's disease.
Alzheimer's, in addition to memory, affects other cognitive areas (Figure 1) and it is common to develop psychiatric symptoms in progression. These symptoms directly affect the patient's functionality and therefore their autonomy.
Currently, there are few drugs that can influence the evolution of the disease: the enzyme acetylcholinesterase inhibitors (rivastigmine, galantamine and donepezil) and memantine. However, it should be noted that patients will receive different symptomatic treatments according to the symptoms they develop: antidepressants and neuroleptics among them.
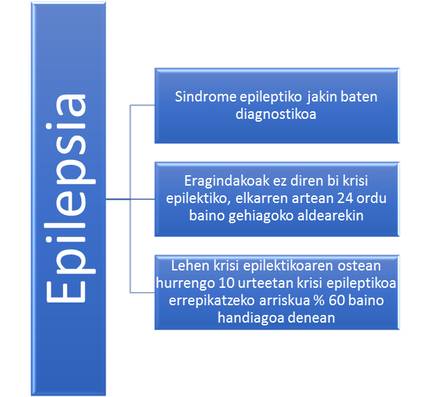
In addition to cognitive and psychiatric symptoms, in recent years the incidence and high prevalence of epileptic seizures in patients with Alzheimer's dementia have attracted attention. It is known that at least 10% of epilepsies are diagnosed to people over 65 years of age, so, as in the case of Alzheimer's, the risk of epileptic seizures and epilepsy (criteria to diagnose as shown in Figure 2) increases with age.
According to some studies, the risk of seizures is between six and ten times higher in patients with Alzheimer's disease than in controls of the same age. In other words, between 1 and 22% of those affected by Alzheimer's dementia will suffer some epileptic seizures (the variability of the figures is due to difficulties in establishing a diagnosis). Consequently, the prevalence of epileptic seizures is considered to be higher than estimated.
Among patients with Alzheimer's dementia, a number of risk factors for seizures have been identified. Among them are the advanced phase of the disease, the disease before the age of 60, Down syndrome, and the most important, Alzheimer's family dementia (by gene mutations of the protein precursor 1 preseniline, 2 or amyloid) or the epileptic activity of the electroencephalogram. For the moment, it has not been shown that memantine and acetylcholinestarase enzyme inhibitors increase the risk of seizures. However, certain symptomatic treatments, including neuroleptics, are known to increase the risk of seizures.
For now, it is not clear what is the pathophysiology of epileptic seizures in Alzheimer's disease. It seems that only the loss of neurons and the resulting atrophy cannot explain the incidence and prevalence of epileptic seizures. Therefore, different stimulating mechanisms (amyloid and tau proteins, calvindine and interleucleukins) have been proposed, but none of them have been demonstrated.
According to published data, the most common types of seizures in these patients (72%) are focal epileptic seizures that cause the disorder of consciousness. In addition, myoclonics of epileptic origin (unwanted rapid muscle agitation) are known to increase the risk of widespread tonic-clonic seizures.
At the moment, the influence of epileptic seizures on the evolution of Alzheimer's disease has not been proven. However, it seems that patients affected by epileptic seizures have worse performance in cognitive assessment tests, especially if these seizures have been generalized tonic-clonic seizures.
As already mentioned, the incidence and prevalence of epileptic seizures may be underestimated by the difficulties we have to diagnose. The first step in establishing the diagnosis is to suspect. Therefore, proper anamnesis is essential for both the patient and, above all, for their caregivers. With clear suspicion, periodic electroencephalograms are not recommended. However, if clearly suspected, this is a test for electroencephalogram.
The alterations that appear in the electroencephalogram (in most cases, temporary focal epileptic activity) should be interpreted along with clinical data, as they may occur between 3 and 6% of Alzheimer's patients without epileptic seizures. Likewise, in 32% of patients with Alzheimer's disease who have suffered epileptic seizures, no alterations will be observed.
Once the diagnosis is made, treatment should be implanted. In patients with Alzheimer's dementia it is recommended to start treatment with anti-epileptic drugs after the first epileptic seizure. As much as possible with a single drug and with the lowest possible dose, as they present a greater risk of suffering the adverse effects of antiepileptics, most associated with the dose, because they are older people and have cognitive alterations. Among the most recommended medications are lamotrigine and levetiracetama. Thanks to treatment, more than 62% of patients manage to be free of epileptic seizures and even more manage to reduce the frequency of seizures.
Finally, the need to know better the incidence and prevalence of epileptic seizures in patients with Alzheimer's dementia. Suspicion is essential to diagnose seizures. Once the diagnosis is made, treatment will be carried out. Looking ahead, the challenge is to better understand the pathophysiology underlying epileptic seizures. It would also be of great interest to know the best evolution of cognition functions in patients treated in time with antiepileptics.
Bibliography
- Friedman Daniel, Lawrence S.Honing, Scarmeas Nikolaos. Seizures and Epilepsy in Alzheimer’s Disease. CNS Neurosci Ther.2012 April;18(4):285-294.
- Irizarry Michael C et al. Incidence of New-Onset seizures in Mild to Moderate Alzheimer Disease. Arch Neurol.2012 March; 69(3):368-372.
- Scharfman, Helen E. “Untagling” Alzheimer’s Disease and Epilepsy. Epilepsy current,Vol 12, No.5 (September/October).2012pp,178-183.
- Pandis Dionysios, Scarmeas Nikolaos. Seizures in Alzheimer's Disease: Date Clinical and Epidemiological. Epilepsy Currents.Vol 12.No.5 (September/October).2012pp,184-187.
- Voseel Keith et al. Seizures and Epileptiform Activity in the Early Stages of Alzheimer Disease. JAMA Neurol. 2013.September 1;70(9):1158-1166.
- Rao Satish C, Dove Gerald, Cascino Gregory D, Ronald C. Petersen. Recurrent seizures in Patients with Dementia: Frequency, seizure-types and Treatment Outcome. Epilepsy Behav. 2009 Jan; 14(1):118-120.
- Cumbo E, Ligori LD. Levetiracetam, lamotrigine, and phenobarbital in patients with epileptic seizures and Alzheimer’s disease. Epilepsy Behav. 17(4) April 2010: 461-6.
- Nicastro Nicolas, Assal Frédéric, Seeck Margita. From here to epilepsy: the risk of seizure in patients with Alzheimer’s disease. Epileptic Disord 2016;18(1):1-12.






