Polymeric biomaterials. Plastics that form the human body
Biomaterials are inert materials designed to interact with biological systems (definition agreed in the “Consensus Conference” BIOMAT 1986).

Biomaterials have a long history, as the functions of tissues and the restoration sessions of the body parts have long been done with natural or artificial materials. A. C. We know that techniques such as: Edgar Smith's papyrus describes wound closure systems and other purposes. A. C. Other works around 2000 indicate that metals were used to repair bones. It has also become known the use of goose feathers to repair blood vessels. This news from a long time ago explains that some steps have been taken on this path and that metals that had already begun to be used seriously in bone repair surgery at the beginning of the last century.
Later, throughout this century, in the 1930s, came the development of the plastics industry, which meant the introduction of polymers in bone repairs. Plastics also began to search for their place among biomaterials. Other things, II. The World War gave great impetus to research in this field. The consequences of the war itself generated the need for implants and extracorpotical devices and the development of materials for industrial use allowed testing the first useful devices. As an example of the benefits for medicine derived from advances for industry, we can cite: Dr. Koff's artificial kidney was the result of the development of a sausage pickup cellophane.

The advances that have taken place in this field in the last 30 years are, without any fear, enormous steps. The table shows a relationship of the main uses of polymers in medicine, and as can be seen, it is a very complete list that covers all fields of medicine. In addition to all this, it is worth noting the huge presence of polymers in the field of orthodontics. Today, orthodon-tecs, and they have said, should close consultations in the absence of polymers.
In addition to these areas that we can already classify as classic, there is a new framework that begins to break the path, that of pharmacology. There are new medicines that use polymers that require a very special role for polymer. On the one hand, it is intended that the dosage of the drug be produced within the body and, on the other, that it only reaches the desired point.
Traumatology is undoubtedly the most widely used medical-surgical specialty in the use of pro-thesis materials of polymer origin. Traumatological accidents are very numerous in the industrial world and in the means of transport, to which we must add degenerative diseases. The vast majority of joint prostheses have some polymeric component. Finger joints are usually replaced by silicone materials, for example.

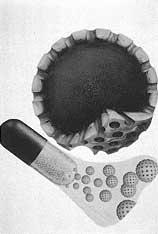
The surgery most applied in this specialty will be, logically, that of the hip and knee joint. In these joints it is often used by combining metal, polyethylene or teflon. In addition, the "cement" used to place these pieces in the body is usually poly(methylmethacrylate). The particularity of the use of these cements is that it is polymerized in the place where the insertion is to be made, so that a complete adaptation to the gap left by the original parts is achieved.
Skin tissue prostheses have also been highly developed. The tegument of the human organism, known as skin or skin, is the organ with the largest body surface and its function is to protect, protect from external agents. The most common skin lesions are scratches, perforations, and burns.
The treatment of injuries caused by burns in these will probably be the most used of polymeric biomaterials. The therapeutic treatment of burns is long and requires protective and bioadhesive layers. However, when you want to promote a regeneration process of skin tissues it is not advisable to use inert materials. It is necessary to use materials that generate hyperreaction in the area. Thus, without losing bioadhesiveness, a huge and rapid growth of cells is achieved. Given these characteristics, several polymeric systems have been used in the last 30 years. The most commonly used are polytetrafluoroethylene (teflone), polypropylene, polyamide (nylon) and poly (ethylene glycol terephthalate) (dracona).
The experimentation of recent years has allowed to use two ways of treatment of burns. The first route is the use of adhesive polymeric biomaterial that fully fits the injury area. The materials used for this technique are those mentioned above. The second route is based on the use of hydrogels. These hydrogels are meshed and inflated hydrophilic polymers in water. We can cite dextrones, polypeptides and collagen as examples of this last group.

Most surgical interventions require some kind of open wound closure material. Although it seems a minor step, the success of the entire intervention lies in its purity and effectiveness. The material used must be a material that maintains mechanical resistance throughout the healing process and produces the least possible reactions (to prevent the generation of debts in the post-operative process).
The healing process is very complex because different types of tissues are played, because as the wound closes the mechanical tension changes, because the suture material must be in contact with different physiological fluids and, ultimately, because surgical wounds can be of various types (with their own characteristics). That is why we must use different materials, depending on the type of wound, the place in which it is located and the criteria of the surgeon.
The main function of a suture is to keep the wound edges in contact. And so you should keep the material used until the body generates the natural collagen necessary for the healing process. As the wound closes and therefore increases the resistance of the regenerated fabrics, it is advisable that the material used for the seam lose resistance. Therefore, the ideal seam must meet the following requirements:
- Be useful, comfortable and natural.
- Minimal tissue reaction.
- Proper tensile strength and safety when performing knots.
- Be anti-allergic, waterproof and inert.
Until a few years ago, natural scrubs have been used for bonfires, such as cotton, silk and catgut (composed of collagen extracted from the ovine submucosa). Today, synthetic materials are gradually gaining ground. These synthetic materials have greater resistance than cotton and silk and less inflammatory reaction than catox.
As a result, polyamide, polypropylene and polyester fibers are replacing the former in operating theatres. Polyester fibers, for example, are used in cardiovascular surgery because they maintain mechanical strength for long periods of time. On the contrary, polypropylene monofilaments are mainly used in abdominal operations, due to their good mechanical strength, safety in the knots, resistance to infections and biocompatibility.
In some applications it is necessary to use a system that allows its absorption by the organism itself. This absorption is usually performed by biodegradable enzyme reactions. Catox has until recently been the main use of these uses, although its tendency to tissue inflammation is known. In recent times new formulations have been developed for application in applications such as poly (glycolic acid), glycolic acid/lactic acid copolymers and polydioxanone. For example, glycolic acid/lactic acid copolymers (also known as polyglactine) has very favorable characteristics for eye surgery, as it produces a very low reaction with eye tissues and a linear loss of resistance after intervention.

We have started with the visual apparatus and we will continue with it, since the contribution of these children in this field of medicine has been very important. The applications of plastic materials in ophthalmology have allowed many people to improve their quality of life, sometimes maintaining vision and improving in many others. Plastic materials have a great tradition in the glasses holders to manufacture lenses (“organic glass”) and contact lenses (both hard and soft).
The advances made in ophthalmology in recent years include intraocular lenses. When cataracts form in the lens of the eye, the lens loses transparency and can eventually become completely dazzled. Visual recovery is possible after surgical removal of the affected eye lens, using glasses or special contact lenses for cataracts.
Both options have or may have discomfort for the patient. For example, if the most appropriate solution is the use of contact lenses, some people may not adapt to their use. Keep in mind that most people who need cataract surgery are older. An English ophthalmologist was the first to apply the permanent intraocular lens of polymethylmethacrylate to a cataract operated person.
Why did you choose this polymer? The reason is: II. In a plane crash in the World War, the pilot was hit with a piece of poly carlina (methylmethacrylate) and doctors were able to verify that there was no rejection. Since then the compatibility of this material with eye tissues was known. The success of such interventions currently exceeds 99%. However, research is underway in this field, testing new plastic materials and surgical techniques.
Finally, we will make one more mention before we finish. Polymeric adhesives are used in the treatment of perforated cornea and ulcers, as well as in corneal prostheses and in retinal surgery.
“We want to do research close to the application”
Interview with Marilo Gurrutxaga and Isabel Goñi, professors and researchers from the Department of Polymer Science and Technology of the Faculty of Chemistry of San Sebastian.
SDGs. In recent years you are immersed in the study of biomaterials. How have you come to this area?
I.G.& M.G. Our initial research focused on the exploitation of biomass in the use of diving slabs. What we did was get vaccine-type copolymers. For this we used starch, one of the most important components of vegetable biomass, and acr-yl polymers. Using starch and similar components and transforming them with synthetic polymers, we obtained degradable copolymers. Acrylic polymers, on the other hand, are very important for their biocompatibility between bioplastics. For years we have worked on a very basic research, that is, on synthesis tasks, especially acrylics. But we did not synthesize it and analyze the exploitation of the materials studied, and we believe that the work done was doomed. This led us into the field of biomaterials, where it was easier to see the applications of the materials used in research and work with a specific objective. We continue with acrylic polymer and starch, but research has a clearer direction.

SDGs. What is your research now?
M.G. & I.G. We are currently working in two areas. On the one hand, with materials for special medicines, i.e. controlled dosage and bioadhesives. And on the other, with acrylic cements for bones. In these two lines we focus now.
SDGs. In 1991 the prestigious Conference on polymeric biomaterials took place in San Sebastian.
M.G. & I.G. Well, it is true that the days that were held in November 1991 had a great importance for us, since we had the opportunity to contact those who were working on this subject. The aim of the conference was to bring together pharmacists, doctors, biologists, chemists and even technologists, since coordination in this field is fundamental. Researchers and doctors need to know each other so that research contributes to real medicine.
Tere Barrenetxea
Polymer Applications in Surgery and Hospital ClinicTemporary devices
Semi-permanent devices
Complex devices with physiological functions
Extracorpotical materials
|





